Introduction: Why Diabetic Retinopathy Matters
Diabetes is one of the fastest-growing health challenges globally, and with it comes a significant risk to eye health. Diabetic Retinopathy (DR) is a diabetes-related complication that damages the blood vessels in the retina, leading to vision problems and, in severe cases, blindness.
According to the World Health Organization, diabetic retinopathy affects 1 in 3 people living with diabetes, making it one of the leading causes of preventable blindness.
What is Diabetic Retinopathy?
Diabetic retinopathy is a progressive eye disease caused by long-term high blood sugar levels. Over time, uncontrolled diabetes damages the delicate blood vessels in the retina (the light-sensitive tissue at the back of the eye), leading to vision problems.
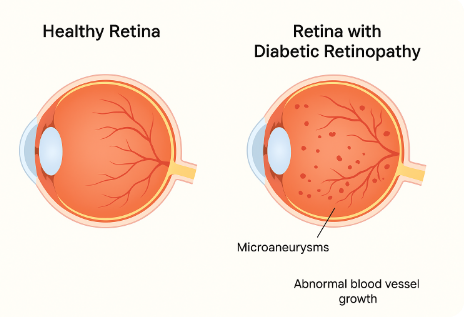
There are two major stages of diabetic retinopathy:
- Non-proliferative diabetic retinopathy (NPDR) – Early stage with weakened blood vessels, microaneurysms, and small leaks.
- Proliferative diabetic retinopathy (PDR) – Advanced stage with abnormal new blood vessel growth that can cause severe vision loss.
Causes and Risk Factors
The primary cause of diabetic retinopathy is chronically high blood sugar levels that damage tiny retinal blood vessels. But several risk factors increase the likelihood of developing the condition:
- Duration of Diabetes: The longer you live with diabetes, the higher your risk.
- Poor Blood Sugar Control: Uncontrolled glucose levels accelerate damage.
- High Blood Pressure & Cholesterol: Both worsen vascular damage.
- Smoking: Nicotine contributes to poor circulation and retinal stress.
- Pregnancy in Diabetic Women: Increases risk of DR progression.
Symptoms of Diabetic Retinopathy
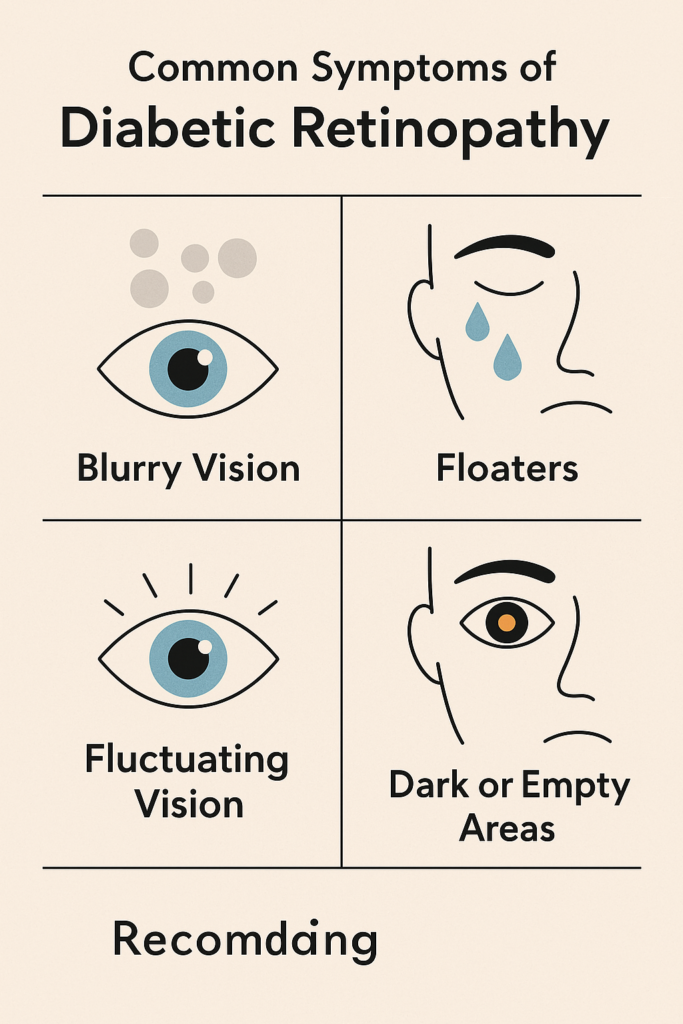
In its early stages, diabetic retinopathy often has no noticeable symptoms, which is why regular eye exams are critical. As the disease progresses, symptoms may include:
- Blurred or fluctuating vision
- Dark spots (floaters) or strings in vision
- Trouble seeing at night
- Colors appearing faded or washed out
- Sudden vision loss in advanced cases
👉“Learn more about floaters and flashes — what’s normal and what could be an emergency.”
Diagnosis: How Is Diabetic Retinopathy Detected?
Eye specialists use several diagnostic tools to detect diabetic retinopathy, often before symptoms appear:
- Dilated Eye Exam – Allows a direct view of the retina.
- Optical Coherence Tomography (OCT) – Scans retinal layers for swelling or damage.
- Fluorescein Angiography – Identifies leaking blood vessels.
- Visual Acuity Test – Measures sharpness of vision.
Prevention Strategies
While not all cases can be prevented, the risk of diabetic retinopathy can be significantly reduced through lifestyle and medical strategies:
- Blood Sugar Control – Keep HbA1c below 7% (or target advised by your doctor).
- Manage Blood Pressure & Cholesterol – Reduces vascular stress.
- Healthy Lifestyle – Eat nutrient-rich foods (antioxidants, omega-3s, leafy greens).
- Regular Exercise – Improves blood circulation and insulin sensitivity.
- Routine Eye Exams – Annual comprehensive eye exams are critical.
👉“Discover how antioxidants like vitamins A, C, and E protect your eyes from damage.”
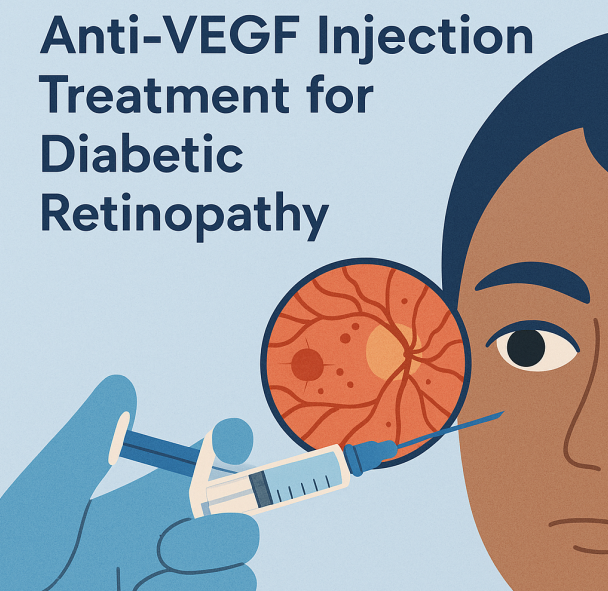
Treatment Options
Treatment depends on the stage of the disease and the severity of damage.
1. Medications
- Anti-VEGF injections (e.g., Avastin, Eylea, Lucentis) reduce abnormal vessel growth.
- Steroid injections may reduce retinal swelling.
2. Laser Therapy (Photocoagulation)
- Seals leaking vessels and shrinks abnormal blood growth.
3. Vitrectomy Surgery
- Removes scar tissue and blood from the vitreous to restore vision.
4. Lifestyle Integration
- Proper diet, exercise, and supplementation to support long-term eye health.
Living with Diabetic Retinopathy
Managing diabetic retinopathy is not just about medical treatments—it’s about lifestyle alignment. Patients should:
- Stick to medication schedules
- Avoid smoking
- Monitor vision changes
- Maintain follow-up visits with ophthalmologists
Frequently Asked Questions (FAQ)
1. Can diabetic retinopathy be cured?
No, but early detection and treatment can slow or stop progression.
2. How often should diabetics get an eye exam?
At least once a year, or more frequently if retinopathy has been diagnosed.
3. Does everyone with diabetes get diabetic retinopathy?
Not necessarily, but the risk increases with poor blood sugar control and duration of diabetes.
4. What’s the biggest risk of untreated diabetic retinopathy?
Permanent vision loss or blindness.
5. Can supplements help protect vision in diabetes?
Yes, antioxidants (vitamins A, C, E), omega-3 fatty acids, and lutein/zeaxanthin support retinal health.
Product Recommendations
💡 Support your eye health with carefully selected vision supplements and protective gear:
- Ocuvite Eye Health Supplements – Rich in lutein, zeaxanthin, and omega-3s.
- Blue Light Blocking Glasses – Reduce strain from screens and protect the retina.
- PlantVital Moringa Capsules – Natural antioxidant powerhouse for eye and overall health.
- Artificial Tears Eye Drops – Keeps eyes hydrated and reduces discomfort.
- Digital Eye Strain Relief Lamp – Adjustable lighting to reduce glare and eye fatigue.
Conclusion
Diabetic retinopathy is one of the most serious eye complications linked to diabetes, but with early detection, prevention, and proper treatment, vision loss can often be delayed or avoided.