Introduction: The Growing Crisis of Diabetic Vision Loss
Diabetes is one of the fastest-growing health challenges globally, and with it comes a significant risk to eye health. Diabetic Retinopathy (DR) is a complication that damages the blood vessels in the retina, potentially leading to total blindness if left unmanaged.
According to the World Health Organization, DR affects 1 in 3 people living with diabetes. In the modern era, where screen time is high and metabolic health is often compromised, understanding the Brain-Eye-Metabolic axis is the first step toward lifelong clarity.
Part 1: Understanding the Stages of Retinal Damage
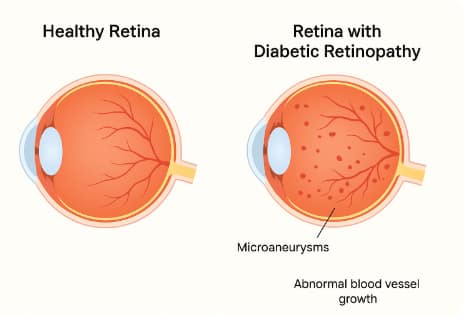
Diabetic Retinopathy is a progressive disease caused by long-term high blood sugar levels. It is generally categorized into two major stages:
1. Non-Proliferative Diabetic Retinopathy (NPDR)
This is the early stage where blood vessels in the retina weaken.
- Microaneurysms: Tiny bulges in the blood vessels that often leak fluid.
- Retinal Edema: Swelling of the retina, which can lead to blurred vision.
- Lipid Deposits: Small “hard exudates” that appear on the retina.
2. Proliferative Diabetic Retinopathy (PDR)
This is the advanced, vision-threatening stage.
- Neovascularization: The body attempts to grow new blood vessels to replace damaged ones, but these new vessels are fragile and abnormal.
- Vitreous Hemorrhage: These abnormal vessels can leak blood into the center of the eye, causing “floaters” or complete vision blockage.
- Tractional Retinal Detachment: Scar tissue from new vessels can pull the retina away from the back of the eye.
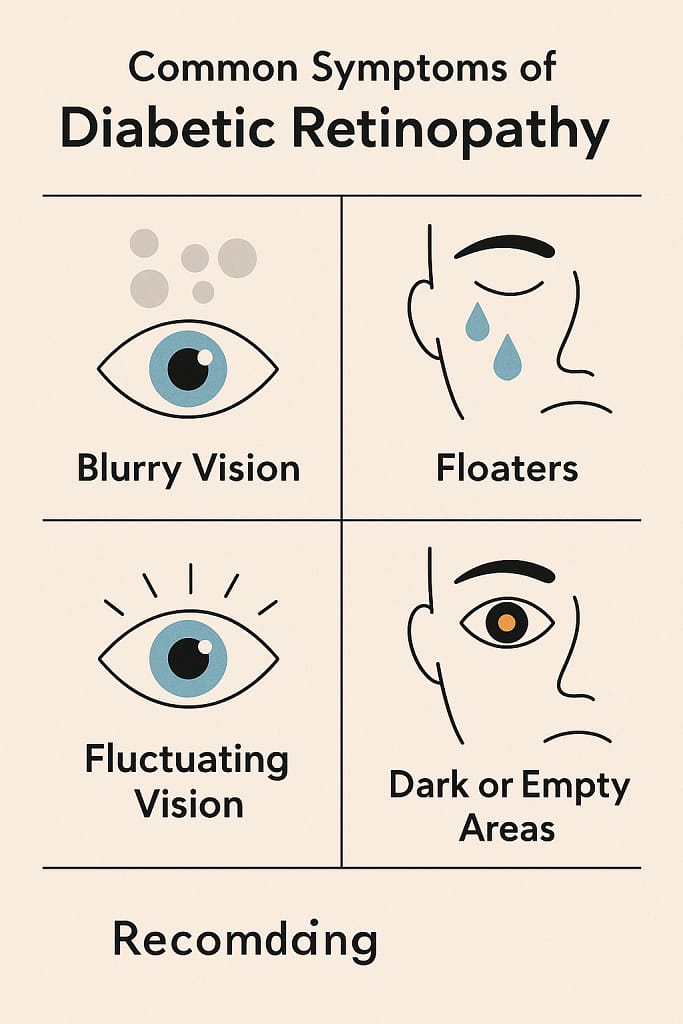
Part 2: Symptoms and The “Silent” Danger
In the early stages, DR often has no noticeable symptoms. This makes regular dilated eye exams critical for early detection. As the condition advances, you may experience:
- Fluctuating Vision: Vision that changes based on your blood sugar levels.
- Floaters: Dark spots or strings that “drift” across your vision.
- Faded Colors: Colors may appear washed out or less vibrant.
- Sudden Vision Loss: Often a sign of a hemorrhage or retinal detachment.
1. The HbA1c Goal & CGM Tracking
Maintaining an HbA1c below 7% is the gold standard.
- Biohack: Use a Continuous Glucose Monitor (CGM) to identify “glucose spikes” after meals. It is these rapid spikes, rather than just the average sugar levels, that do the most damage to the delicate retinal capillaries.

Precision Glucose Monitor Kit
The first step in preventing Diabetic Retinopathy is eliminating glucose spikes. This clinical-grade monitor protects your retinal capillaries from oxidative damage.
2. Ocular-Specific Nutrition
Beyond general health, specific nutrients act as “vascular shields” for the retina:
- Benfotiamine (Vitamin B1): Helps block the pathways that allow high sugar to damage blood vessels.
- R-Alpha Lipoic Acid: A powerful antioxidant that can cross the blood-retinal barrier to protect mitochondria.
- Lutein & Zeaxanthin: Protect the macula from oxidative stress caused by blue light, which can worsen diabetic retinal inflammation.
3. Blood Pressure & Cholesterol Management
High blood pressure and high cholesterol both worsen vascular damage in the eye. Maintaining a blood pressure of 120/80 mmHg or lower is crucial for preventing vessel leakage.
Treatment Options
Treatment depends on the stage of the disease and the severity of damage.
1. Medications
- Anti-VEGF injections (e.g., Avastin, Eylea, Lucentis) reduce abnormal vessel growth.
- Steroid injections may reduce retinal swelling.
2. Laser Therapy (Photocoagulation)
- Seals leaking vessels and shrinks abnormal blood growth.
3. Vitrectomy Surgery
- Removes scar tissue and blood from the vitreous to restore vision.
4. Lifestyle Integration
- Proper diet, exercise, and supplementation to support long-term eye health.
While glucose control is the foundation, targeted vascular antioxidants can act as a secondary shield for your eyes. Scientific research suggests that specific nutrients can bypass the blood-retinal barrier to neutralize the oxidative stress that leads to permanent vision loss

Benfotiamine + ALA
Engineered to block high-sugar damage and shield retinal capillaries.
Living with Diabetic Retinopathy
Managing diabetic retinopathy is not just about medical treatments—it’s about lifestyle alignment. Patients should:
- Stick to medication schedules
- Avoid smoking
- Monitor vision changes
- Maintain follow-up visits with ophthalmologists
Clinical guidelines and screening recommendations are provided by the American Academy of Ophthalmology .
Frequently Asked Questions (FAQ)
1. Can diabetic retinopathy be cured?
No, but early detection and treatment can slow or stop progression.
2. How often should diabetics get an eye exam?
At least once a year, or more frequently if retinopathy has been diagnosed.
3. Does everyone with diabetes get diabetic retinopathy?
Not necessarily, but the risk increases with poor blood sugar control and duration of diabetes.
4. What’s the biggest risk of untreated diabetic retinopathy?
Permanent vision loss or blindness.
5. Can supplements help protect vision in diabetes?
Yes, antioxidants (vitamins A, C, E), omega-3 fatty acids, and lutein/zeaxanthin support retinal health.
Conclusion: Vision is a Metabolic Choice
Diabetic retinopathy is a serious condition, but it is not an inevitable fate. By moving beyond simple sugar control and embracing Vascular Biohacking—using CGMs, targeted antioxidants, and regular screenings—you can protect your retina for a lifetime. Your vision is a reflection of your metabolic health; fuel it wisely.Conclusion
Diabetic retinopathy is one of the most serious eye complications linked to diabetes, but with early detection, prevention, and proper treatment, vision loss can often be delayed or avoided.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."



