Keratoconus is a progressive eye condition that occurs when the normally round cornea (the clear front surface of the eye) becomes thin and begins to bulge into a cone-like shape. This irregular shape deflects light entering the eye, causing distorted vision. Although rare, keratoconus is one of the leading causes of corneal transplants worldwide, making early detection and treatment critical for long-term vision health.
In this article, we’ll explore the causes of keratoconus, early signs to look for, and available vision correction options — from glasses and contact lenses to advanced surgical procedures.
What is Keratoconus?
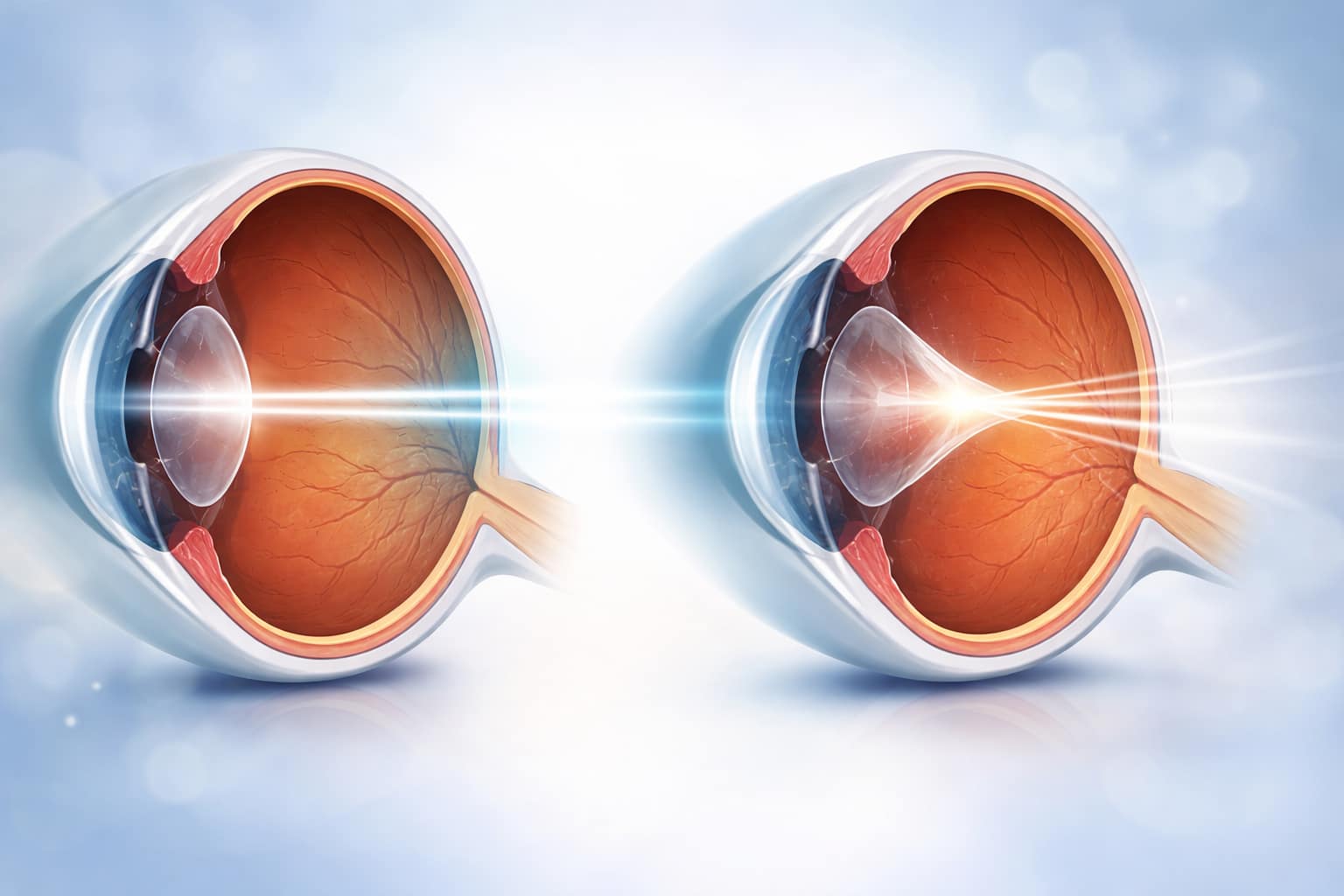
The cornea plays a vital role in focusing light onto the retina. In keratoconus, the cornea gradually thins and weakens, which leads to protrusion into a cone shape. This abnormal curvature prevents light rays from focusing correctly, resulting in blurry and distorted vision.
Unlike many eye conditions that stabilize over time, keratoconus often progresses, especially in younger patients. It typically affects both eyes, although severity can differ between them.
Causes of Keratoconus
While the exact cause of keratoconus is not fully understood, several risk factors and potential contributors have been identified:
- Genetic Predisposition – Family history increases the risk. About 10% of keratoconus patients have a relative with the condition.
- Chronic Eye Rubbing – Aggressive or habitual eye rubbing may contribute to corneal thinning.
- Underlying Health Conditions – Certain conditions such as Down syndrome, asthma, and connective tissue disorders have been linked to keratoconus.
- Oxidative Stress – Imbalances between free radicals and antioxidants may damage corneal tissue.
💡 Did you know? Eye rubbing after waking or before sleep can increase pressure inside the eye up to 20 times normal levels — enough to accelerate corneal deformation in vulnerable individuals.
Early Signs and Symptoms
Keratoconus often begins during adolescence or early adulthood and progresses over 10–20 years. Early detection can significantly improve treatment outcomes.
Common Symptoms:
- Blurred or distorted vision
- Increased sensitivity to light and glare
- Frequent changes in eyeglass prescriptions
- Difficulty seeing at night
- Eye strain or headaches
In more advanced stages, patients may experience sudden worsening of vision due to corneal scarring or swelling (hydrops).

Vision Correction Options for Keratoconus
Treatment depends on the severity of the condition and how quickly it progresses. Early stages can often be managed with corrective lenses, while advanced cases may require surgical interventions.
1. Glasses and Soft Contact Lenses
- Useful in the very early stages.
- As keratoconus progresses, these options may no longer provide adequate vision correction.
2. Rigid Gas Permeable (RGP) Lenses
- Hard contact lenses that mask the irregular corneal shape.
- Provide clearer vision by creating a smooth refracting surface.
3. Hybrid and Scleral Lenses
- Hybrid lenses combine a rigid center with a soft outer skirt for comfort.
- Scleral lenses vault over the cornea and rest on the sclera (white part of the eye), providing stability and sharp vision.
4. Corneal Cross-Linking (CXL)
- A minimally invasive procedure that strengthens corneal tissue by applying riboflavin drops and UV light.
- Proven to halt or slow the progression of keratoconus.
5. Intacs (Intracorneal Ring Segments)
- Tiny arc-shaped inserts placed within the cornea.
- Flatten the cornea to reduce irregularity and improve vision.
6. Corneal Transplant (Keratoplasty)
- Considered in advanced keratoconus with significant scarring or vision loss.
- Options include partial-thickness (DALK) or full-thickness (PK) transplants.

Lifestyle and Preventive Measures
- Avoid excessive eye rubbing.
- Manage allergies to reduce irritation.
- Schedule regular eye exams for early detection.
- Use protective eyewear in sports or high-risk activities.
💡 Did You Know?
A 2024 study found that patients who used nutritional supplements rich in Vitamin C and lutein had a 17% slower progression of corneal thinning compared to those who didn’t.

Preservative-Free Relief Drops
Prevent the urge to rub your eyes—the leading cause of Keratoconus progression—with soothing, sterile drops.
Shop Eye Relief →Living with Keratoconus
With early diagnosis and appropriate treatment, most individuals with keratoconus can maintain good vision and quality of life. Modern innovations such as scleral lenses and corneal cross-linking have significantly reduced the need for corneal transplants.
Keratoconus: Frequently Asked Questions
1. Can this condition go away on its own?
No. It is a progressive disorder that usually worsens without medical intervention. However, modern treatments like cross-linking can effectively stop or slow down the thinning process.
2. Are standard contact lenses an option?
Generally, no. Because the cornea becomes irregular in shape, standard soft lenses won’t fit properly and often provide poor vision. Specialized options like scleral or RGP lenses are typically required for clear sight.
3. Is there a genetic link?
Yes, genetics play a significant role. If a close relative has been diagnosed with Keratoconus, it is highly recommended to schedule regular screenings to catch early signs.
4. Can LASIK fix the distorted vision?
No. In fact, laser surgeries like LASIK are dangerous for people with this condition because they involve removing corneal tissue, which further weakens the already thin surface.
5. What is the success rate of stabilization surgery?
Corneal cross-linking is highly effective, with over a 90% success rate in halting disease progression and stabilizing the eye’s structure within the first year.
✅ Conclusion
Keratoconus is a challenging but manageable eye condition. By understanding the causes, recognizing the early signs, and exploring treatment options, patients can take control of their vision health. If you suspect keratoconus or experience rapid changes in your eyesight, consult an eye specialist promptly.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."