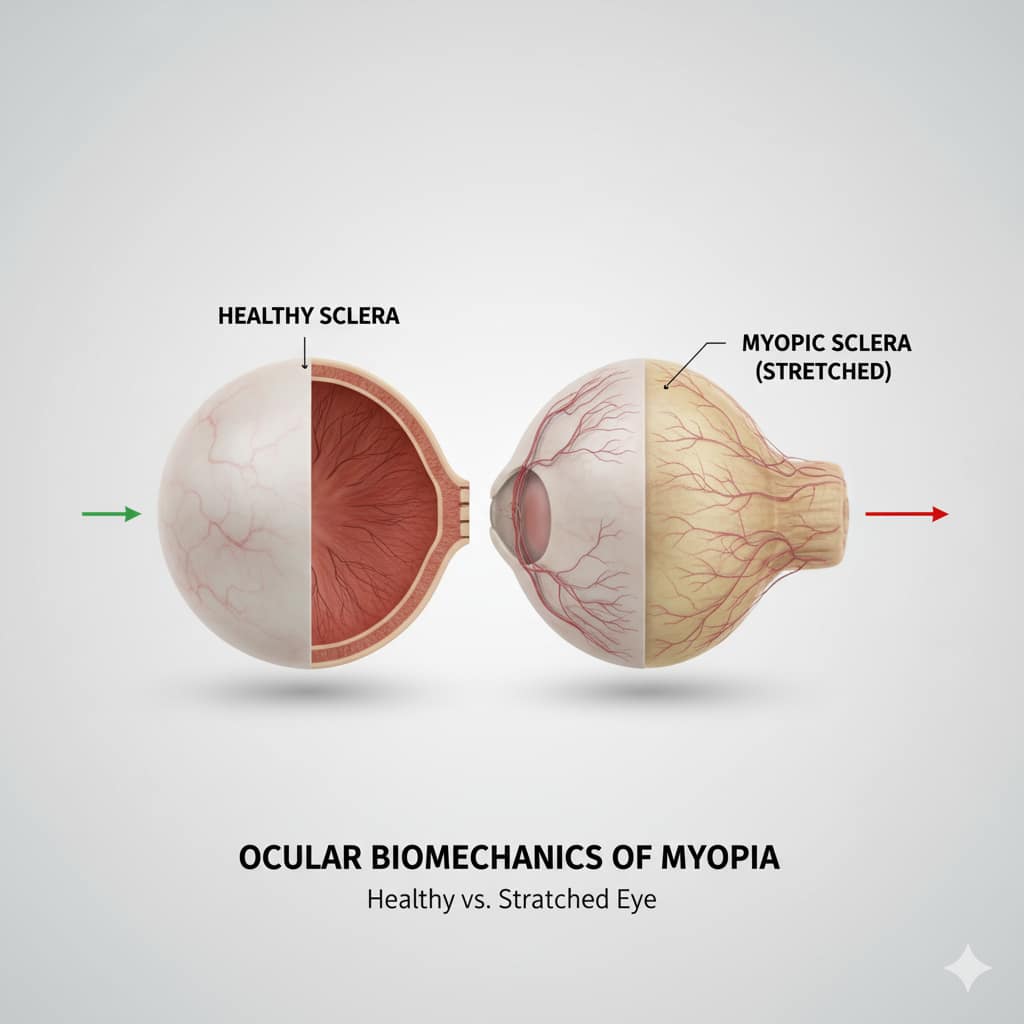
The global rise of nearsightedness is directly tied to the mechanical stresses we place on the eye. Understanding the Ocular Biomechanics of Myopia is the critical first step in controlling this epidemic. For too long, myopia was simply treated as a refractive error—a simple focusing problem fixed with stronger glasses. However, modern research reveals a far more serious underlying issue: a mechanical failure. Myopia progression is fundamentally driven by the science of the ocular biomechanics of the eye, specifically the uncontrollable stretching of the posterior sclera and axial elongation.
This definitive guide delves into the advanced scientific and biomechanical truths behind myopia. We will explore the collagen matrix, the role of mechanical stress, and how cutting-edge research is targeting the eye’s physical structure—not just its optics—to halt progression. If you are a parent seeking to protect your child’s long-term vision, or a specialist looking to understand the next frontier of myopia control, grasping the Ocular Biomechanics of Myopia is essential.

PREMIUM LED EYE THERAPY DEVICE — Instant Strain Relief
Get 20% OFF exclusive to Clear Vision Tips readers!
1. Defining the Problem: The Biomechanical Basis of Myopia
Myopia is not a static condition; it is a progressive, structural disorder. The increase in prescription power is merely a symptom of the eye physically stretching and elongating along its central axis.
Axial Elongation vs. Refractive Myopia
- Axial Elongation: This is the primary driver of pathological myopia. It refers to the abnormal increase in the length of the eyeball (the distance from the cornea to the retina). For every millimeter the eye lengthens past the healthy norm, the risk of serious complications (such as retinal detachment or myopic macular degeneration) increases exponentially. Ocular Biomechanics of Myopia is the study of the forces that cause this stretching.
- Refractive Myopia: This is less common and results from an abnormally steep curvature of the cornea or lens, where the axial length remains normal.
The Critical Role of the Sclera in Progression
The sclera (the white, tough outer wall of the eye) is the central focus of biomechanical research. In progressive myopia, the scleral tissue becomes weakened, thinned, and less rigid due to degradation of the collagen fibers that provide its structural integrity.
- Mechanical Stress: Prolonged near-work and specific visual signals create biomechanical stress on the posterior pole of the eye. If the sclera lacks rigidity, it yields to this stress, leading to permanent elongation. Therapeutic interventions are increasingly focused on stabilizing or strengthening this tissue.
Did You Know?
Myopia progression isn’t just about poor focusing—it’s about the eye physically stretching. The entire field of **Ocular Biomechanics of Myopia** focuses on how to strengthen the sclera (the tough outer wall of the eye) to resist this stretching, which is the primary cause of high myopia and associated vision risks.
2. The Structural Components of Myopia Progression
To combat the condition, we must understand the tissue at a cellular and molecular level. The Ocular Biomechanics of Myopia is heavily dependent on the composition of the Extracellular Matrix (ECM) of the sclera.

Collagen and Extracellular Matrix Degradation
The sclera is primarily composed of Type I Collagen. In myopic eyes, the sclera displays several abnormalities:
- Collagen Fibril Disorganization: The collagen fibers become thinner and irregularly arranged, leading to less structural strength.
- Altered Ratios: There is a decreased ratio of Type I to Type V collagen, further compromising the tissue’s ability to resist stretching forces.
- ECM Remodeling: Enzymes like Matrix Metalloproteinases (MMPs) are thought to be overexpressed in the myopic sclera, actively breaking down the ECM components, contributing directly to thinning and elongation.
Changes in Choroidal Thickness and Blood Flow
The choroid—the vascular layer beneath the retina—also plays a critical biomechanical role. It acts as a mechanical cushion and provides essential nourishment to the outer retina.
- Choroidal Thinning: In progressive myopia, the choroid often thins significantly. This thinning is correlated with axial elongation and is thought to reduce the cushioning effect, making the eye more susceptible to biomechanical stress and structural damage.
3. Advanced Diagnosis and Monitoring
Traditional eye exams focus only on visual acuity (the Snellen chart). Modern myopia control requires precise measurement of the eye’s physical dimensions to assess the actual biomechanical risk.
Ocular Biomechanics of Myopia: Using Axial Length Measurement
Axial length (AL) measurement is the single most critical biometric parameter in modern myopia management.
- Biometry Devices: Devices like the IOLMaster or Lenstar use partial coherence interferometry to measure AL with sub-micron accuracy.
- Monitoring Progression: Instead of just tracking diopters (which can fluctuate), specialists now track the rate of AL growth (e.g., in mm/year). Stopping AL growth is the primary goal of any therapeutic intervention targeting the Ocular Biomechanics of Myopia.
Topography and Biometry in Pediatric Exams
- Corneal Topography: Provides a detailed map of the corneal curvature, helping rule out refractive myopia and aiding in the fitting of Orthokeratology (Ortho-K) lenses, which exert their own biomechanical influence on the cornea.
- Prediction Modeling: New tools use initial AL and corneal power to predict the child’s final adult axial length, allowing specialists and parents to proactively choose the most aggressive necessary intervention.
4. Therapeutic Targets: Intervening in Biomechanics
Current and future treatments are designed specifically to counteract the biomechanical weakness driving the elongation process, either by altering optical signals or by directly stabilizing the scleral tissue.
Pharmacological Strategies (Atropine’s Scleral Mechanism)
While initially thought to primarily paralyze accommodation, low-dose Atropine’s primary efficacy in myopia control is now believed to be biomechanical.
- Scleral Reinforcement: Atropine appears to modulate the biochemical signaling pathways (potentially involving the retina, choroid, and sclera) that regulate scleral growth and remodeling. It may stabilize the ECM by modulating growth factors (like TGF-β) and reducing the enzyme activity (MMPs) that degrades the scleral collagen.
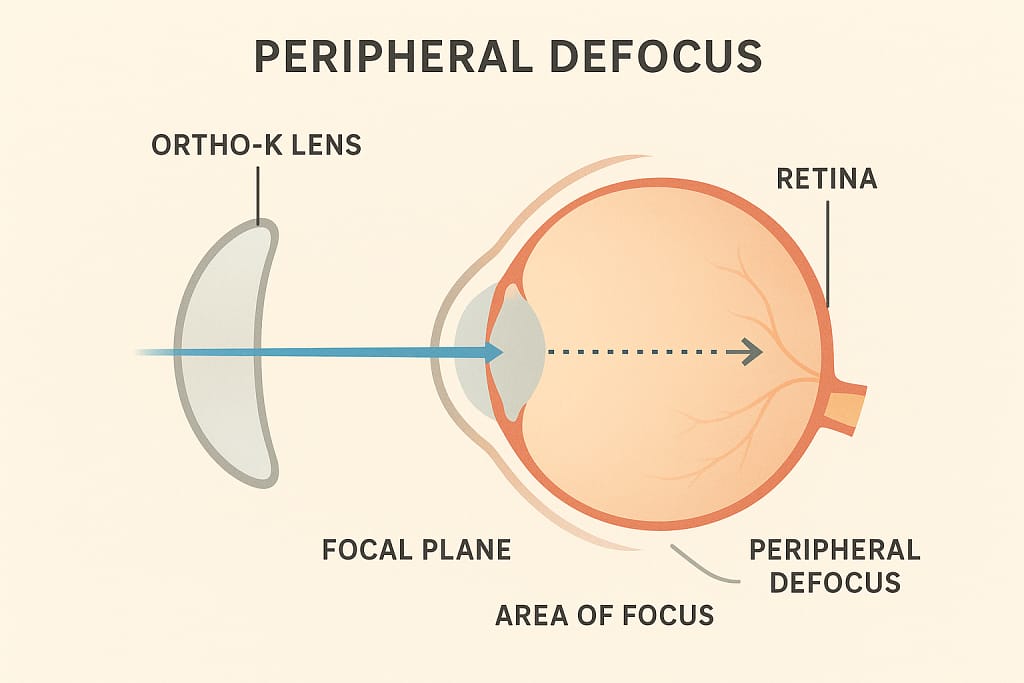
Optical Strategies (Ortho-K, Peripheral Defocus Lenses)
These lenses use precisely engineered optics to alter how light signals reach the peripheral retina, thereby managing the biomechanical signals that stimulate axial growth.
- Peripheral Myopic Defocus: Traditional glasses correct the central vision but cause light to focus behind the peripheral retina, which is thought to signal the eye to stretch further (hyperopic defocus). Myopia control lenses (MiSight, Stellest, Ortho-K) correct the central vision but intentionally focus light in front of the peripheral retina, creating a “myopic defocus” signal that biomechanically tells the eye to stop growing.
5. Future of Intervention: Biohacking the Sclera
The ultimate goal in controlling the Ocular Biomechanics of Myopia is to directly increase the rigidity and strength of the scleral tissue, thereby physically preventing axial elongation. This new frontier is often termed “Vision Biohacking.”

Scleral Cross-Linking and Strengthening Research
Borrowing concepts from corneal cross-linking (used to treat keratoconus), researchers are developing methods to strengthen the posterior sclera. This procedure typically involves:
- Riboflavin and UVA Light: Applying a riboflavin solution to the sclera, followed by controlled exposure to UVA light. This process creates new bonds between collagen fibers, increasing the tissue’s stiffness and resistance to stretching forces.
- Biomechanical Stabilisation: If successful, Scleral Cross-Linking would offer a permanent biomechanical solution, making the eye structurally less likely to elongate, thus halting the progression of high Ocular Biomechanics of Myopia.
Nutritional Biomechanic Support
The synthesis and maintenance of healthy scleral collagen require specific cofactors and nutrients. Nutritional strategies focus on providing the building blocks for a strong Extracellular Matrix (ECM):
- Vitamin C and Copper: Essential cofactors for the enzymes (like lysyl oxidase) that cross-link collagen fibers, which is vital for scleral strength.
- Anthocyanins and Antioxidants: Found in dark berries (like bilberries), these compounds may help protect the scleral tissue from oxidative stress and reduce inflammatory breakdown of the ECM.
Pharmacogenomics in Myopia Control
As treatments become more refined, pharmacogenomics—the study of how genes affect a person’s response to drugs—is poised to revolutionize the treatment of the Ocular Biomechanics of Myopia.
- Personalized Atropine Dosing: Genetic markers may soon allow specialists to predict which children will respond best to low-dose Atropine, and at what specific concentration, optimizing the drug’s biomechanical stabilizing effect from the outset.
6. The Environmental Biomechanical Balance
Environmental factors, while seemingly simple, exert a powerful biomechanical influence on the developing eye. They do not just cause visual fatigue; they directly influence the scleral growth signals.
Outdoor Time: Reducing Biomechanical Stress
Outdoor time is the most proven non-pharmacological intervention for preventing myopia. The mechanism is now understood to be biomechanical and biochemical:
- Dopamine Release: High-intensity ambient light outdoors triggers the release of Dopamine from the retina. Dopamine acts as a powerful inhibitory signal, suppressing the growth factors that tell the sclera to stretch and elongate.
- Light Spectrum: The full, bright spectrum of sunlight provides a more powerful and protective signal to the retina than dim, indoor light, directly counteracting the biomechanical signals of axial elongation.
The Critical Near-Work Distance and Accommodation
Sustained, close-focus tasks create significant biomechanical stress on the eye.
- Accommodation and Vergence: Focusing at near distances requires intense muscular effort (accommodation) and inward turning of the eyes (vergence). This sustained effort increases intraocular pressure and alters the biomechanical tension at the posterior pole, encouraging stretching. Maintaining a healthy working distance (40 cm+) is essential.
Ergonomics and Visual Stress Reduction
Poor ergonomic setups contribute to the biomechanical stress of near-work.
- Screen Position: Laptops and tablets should be positioned to encourage a slight downward gaze, which naturally relaxes the eye muscles (accommodation) and reduces ocular surface exposure, minimizing strain and biomechanical demands.
7. The Link to High Myopia Complications
The most compelling reason to focus on the Ocular Biomechanics of Myopia is to prevent the blinding complications associated with high myopia (typically -5.00 D or greater), which result directly from the stretched tissue.
Retinal Detachment Risk and Biomechanics
As the eyeball elongates, the fixed retina is stretched and pulled taut over a larger surface area. This stretching makes the retina thinner and more prone to tears and holes, dramatically increasing the risk of Retinal Detachment—an ocular emergency. Controlling axial length is the only way to mitigate this biomechanical stress.
Myopic Macular Degeneration (MMD)
MMD is the leading cause of irreversible vision loss in highly myopic individuals.
- Choroidal and Retinal Atrophy: The stretching causes mechanical damage (atrophy) to the central retina and underlying choroid, leading to central vision loss. Controlling the axial length through biomechanical intervention is the primary preventative strategy for MMD.
The Importance of Lifetime Monitoring
Patients with any degree of myopia, especially those with high axial length, require lifelong comprehensive monitoring beyond standard check-ups. This must include:
- Annual Axial Length Measurements: To track stability.
- Peripheral Retinal Examination: To screen for early signs of stretching or detachment risk.
Frequently Asked Questions (FAQ) about Ocular Biomechanics of Myopia
- Q: What is the single most important measurement for Myopia Control?
- A: Axial length (AL). While prescription (diopters) is important for vision clarity, AL (measured in millimeters) is the direct biomechanical indicator of risk for complications like Retinal Detachment and MMD. The goal of all modern treatments is to stop or slow the growth of AL.
- Q: Does wearing weaker glasses slow down myopia?
- A: No. Wearing under-corrected glasses can actually accelerate myopia progression, as it forces the eye to accommodate more intensely, which adds to the biomechanical stress and signals the eye to stretch further.
- Q: Is outdoor time effective even if my child is already myopic?
- A: Yes, absolutely. Outdoor time (ideally 90-120 minutes per day) is effective for both preventing the onset of myopia and for slowing the progression of existing myopia by releasing retinal dopamine, a key inhibitor of axial elongation.
- Q: How quickly should axial length increase in a child?
- A: In non-myopic children, axial length should increase minimally (around 0.1 mm per year). In myopic children, growth exceeding 0.3 mm per year is often considered rapid progression, demanding immediate and aggressive biomechanical intervention.
Conclusion: A Biomechanical Approach to Vision Control
The era of simply prescribing stronger glasses for nearsightedness is over. The science of the Ocular Biomechanics of Myopia provides a clear, actionable roadmap for intervention, proving that we can stabilize the eye’s physical structure. By integrating precise axial length monitoring, pharmacologically stabilizing the sclera (Atropine), employing biomechanically corrective optics (Ortho-K, DIMS lenses), and leveraging environmental controls (outdoor light), we move from managing symptoms to protecting the long-term health and structural integrity of the eye. The future of myopia management is structural, preventative, and ultimately, biomechanical.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."