Introduction
Your eyes are among the most delicate organs in your body, and the retina plays a vital role in capturing light and sending visual information to your brain. One of the most serious conditions affecting this part of the eye is retinal detachment. If left untreated, retinal detachment can lead to permanent vision loss.
In this article, we will cover everything you need to know about retinal detachment, including its early symptoms, causes, risk factors, treatment options, and prevention strategies.
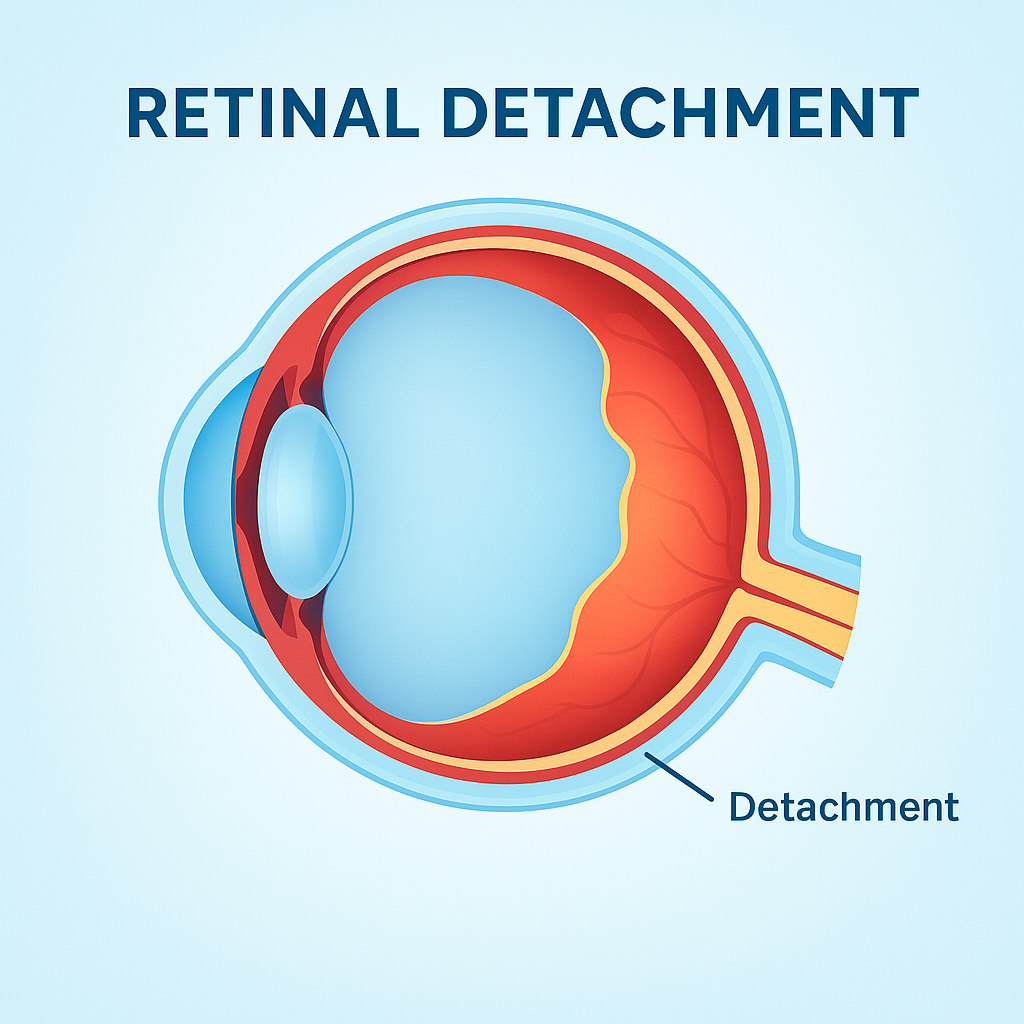
What Is Retinal Detachment?
The retina is a thin layer of light-sensitive tissue lining the back of the eye. Retinal detachment occurs when this layer pulls away from its normal position. Because the retina cannot function properly when detached, vision becomes blurred, distorted, or lost entirely.
There are three main types:
- Rhegmatogenous Retinal Detachment – caused by a tear or hole in the retina.
- Tractional Retinal Detachment – caused by scar tissue pulling on the retina, often linked to diabetes.
- Exudative Retinal Detachment – caused by fluid accumulation beneath the retina, without a tear.
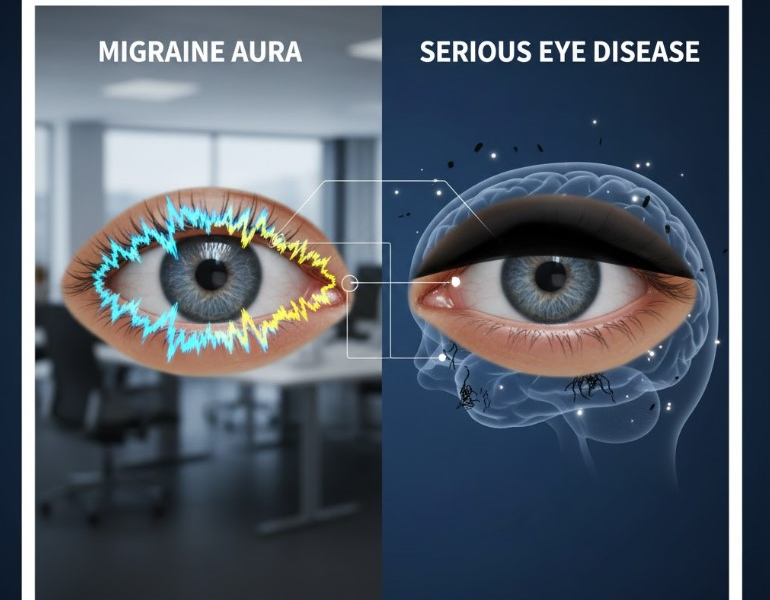
Early Warning Signs of Retinal Detachment
Detecting symptoms early can save your vision. Common warning signs include:
- Sudden appearance of floaters (tiny specks or cobweb-like shapes moving across your vision)
- Flashes of light in one or both eyes
- Blurred or distorted vision
- Dark shadow or curtain moving across your field of vision
- Sudden loss of peripheral vision
If you notice these symptoms, seek emergency medical attention immediately.
Did You Know?
- Every year, nearly 1 in 10,000 people experience retinal detachment — most commonly after age 50.
- If treated within 24 hours of symptoms, over 90% of patients retain useful vision.
- High myopia increases retinal detachment risk up to 10 times compared to normal eyesight.
Causes and Risk Factors
Several conditions increase the likelihood of retinal detachment:
- Aging – retinal thinning is common in people over 50.
- Severe myopia (nearsightedness) – stretches the retina, making tears more likely.
- Eye injury – trauma can cause retinal tears.
- Previous eye surgery – such as cataract removal.
- Family history – genetics plays a role.
- Other eye conditions – diabetic retinopathy, lattice degeneration, or uveitis.
Diagnosis of Retinal Detachment
An ophthalmologist will use:
- Dilated eye exam to check the retina directly.
- Ophthalmoscopy to look for tears or detachment.
- Ultrasound imaging if the retina cannot be seen clearly due to bleeding or cataracts.
Treatment Options
The sooner treatment is started, the greater the chance of saving vision. Common procedures include:
- Laser Photocoagulation – seals retinal tears with a laser.
- Cryopexy (Freezing Treatment) – freezes and reattaches the retina.
- Pneumatic Retinopexy – injecting a gas bubble into the eye to push the retina back.
- Scleral Buckling – a silicone band is placed around the eye to reduce traction.
- Vitrectomy – removal of vitreous gel to relieve pulling forces.
Recovery and Prognosis
Recovery time depends on the severity and treatment method. Many patients regain most of their vision if treated promptly, but delayed treatment can lead to partial or permanent blindness.
Prevention Strategies
While not all detachments can be prevented, you can lower your risk:
- Regular eye exams (especially after 40).
- Protective eyewear during sports or work to prevent injury.
- Controlling diabetes and blood pressure.
- Reporting any sudden changes in vision immediately.
Living With Retinal Detachment
Patients who have undergone treatment may need lifestyle adjustments:
- Avoid heavy lifting or high-impact activities for several weeks.
- Sleep in certain positions if instructed (especially after gas bubble surgery).
- Attend all follow-up appointments.
- Use prescribed eye drops to reduce inflammation and infection risk.
Frequently Asked Questions (FAQ)
Can retinal detachment cause permanent blindness?
Yes. If left untreated, retinal detachment can lead to irreversible vision loss. Early treatment offers the best chance for recovery.
What’s the first sign of retinal detachment?
Sudden flashes of light, new floaters, or a shadow moving across your vision are common early signs. Seek immediate medical attention.
Is retinal detachment painful?
No, it’s usually painless — which makes it even more dangerous because symptoms may be ignored until it’s too late.
Can retinal detachment be prevented?
Not entirely, but regular eye exams, diabetes management, and protecting your eyes from trauma can significantly lower risk.
How long is recovery after retinal detachment surgery?
Depending on the type of surgery, full recovery may take 4–8 weeks. Most patients regain stable vision with proper follow-up care.
Conclusion
Retinal detachment is a medical emergency. Recognizing the warning signs early and seeking treatment quickly can make the difference between saving or losing your vision. With modern treatments, many people can restore functional vision and maintain quality of life.