The experience of chronic, severe dry eye often transcends simple environmental irritation. When standard over-the-counter drops fail, the root cause may lie deep within the body’s immune system. Understanding the link between Sjögren’s Syndrome and Dry Eye is the first step toward effective management. Sjögren’s is a complex, chronic autoimmune disorder that systematically attacks the exocrine glands responsible for producing moisture, leaving the eyes, mouth, and other mucous membranes severely desiccated.
This definitive guide is designed for patients and specialists alike, providing a rigorous, research-backed exploration of this challenging condition. We will delve into the autoimmune mechanisms, detail the cutting-edge diagnostic criteria, and thoroughly examine the advanced pharmacological and procedural interventions—moving far beyond conventional artificial tears—to achieve sustained comfort and protect long-term vision health.
1. The Science Behind Sjögren’s Syndrome and Dry Eye
The dry eye experienced by Sjögren’s patients is not merely a quantitative deficit of tears (aqueous deficiency); it is a disease of systemic inflammation and destruction.
The Autoimmune Mechanism: How Lymphocytes Attack Exocrine Glands
Sjögren’s Syndrome involves a complex, dysregulated immune response where the body’s own T- and B-lymphocytes mistakenly infiltrate and destroy the lacrimal (tear-producing) and salivary glands.
- Inflammatory Cycle: This lymphocytic infiltration leads to chronic inflammation and permanent damage (fibrosis) of the glands, severely diminishing their ability to function. The resulting tears that are produced are of poor quality and highly inflammatory.
- Ocular Surface Damage: The inadequate tear film leads to rapid evaporation and hyperosmolarity (excessive saltiness) of the tear surface. This hyperosmolarity is toxic to the corneal and conjunctival epithelial cells, causing persistent pain, foreign body sensation, and increased risk of corneal ulcers and infections. This is the hallmark of Sjögren’s Syndrome and Dry Eye severity.
The Two Types of Sjögren’s: Primary vs. Secondary
The clinical classification is crucial for systemic management:
- Primary Sjögren’s Syndrome (pSS): Occurs alone, without the presence of another connective tissue disease.
- Secondary Sjögren’s Syndrome (sSS): Occurs alongside another systemic autoimmune disease, most commonly Rheumatoid Arthritis (RA) or Systemic Lupus Erythematosus (SLE). This often complicates treatment, requiring intense coordination between the ophthalmologist and the rheumatologist.
Did You Know?
The lack of tear production in Sjögren’s Syndrome is not just a fluid issue—it’s an **inflammatory** one. The FDA-approved drops like Restasis and Xiidra work by targeting the inflammation caused by the underlying **autoimmune attack** on the lacrimal glands, making them cornerstone treatments for managing chronic **Sjögren’s Syndrome and Dry Eye**.

2. Diagnosis: Moving Beyond Simple Dry Eye
The diagnosis of Sjögren’s Syndrome and Dry Eye requires a comprehensive, multi-step approach that distinguishes it from common forms of dry eye caused by screen use or environment.
Schirmer’s Test and Ocular Surface Staining
While simple, the Schirmer’s Test remains a foundational measurement, quantifying the amount of aqueous tear production.
- Schirmer’s Test: A filter paper strip is placed in the lower eyelid for five minutes. Low wetting (typically less than 5 mm) strongly suggests aqueous deficiency.
- Ocular Surface Staining: Dyes like Lissamine Green and Fluorescein are used to reveal the extent of epithelial damage. Severe staining of the cornea and conjunctiva, particularly the lower third of the cornea, is highly indicative of the severe desiccation seen in Sjögren’s Syndrome and Dry Eye.
Specialized Blood Tests and Diagnostic Criteria
Definitive diagnosis relies on serological testing and specific criteria established by organizations like the American-European Consensus Group (AECG) or the American College of Rheumatology (ACR):
- Autoantibody Testing: Key diagnostic markers include the presence of Anti-SSA/Ro and Anti-SSB/La autoantibodies. The presence of these markers confirms the autoimmune nature of the disease.
- Salivary Gland Biopsy: In uncertain cases, a biopsy of the minor salivary glands (lip biopsy) may be performed to confirm the presence of lymphocytic infiltration.
Sjögren’s Symptom Checker
Assess your symptoms in 30 seconds
*This is not a medical diagnosis. Please consult a specialist.
3. Pharmacological Treatments for Chronic Ocular Disease
Treatment for Sjögren’s Syndrome and Dry Eye must move beyond palliative relief to target the underlying ocular inflammation and dysfunction.
Immunosuppressive Drops (Restasis, Xiidra)
These medications are the first-line pharmaceutical defense against the chronic inflammation driving the disease:
- Cyclosporine A (e.g., Restasis, Cequa): These drops suppress the T-cell activation that leads to glandular destruction and ocular surface inflammation. They aim to break the vicious cycle of inflammation, allowing the lacrimal glands to recover some function over several months.
- Lifitegrast (e.g., Xiidra): This medication works by blocking the interaction of a cell surface protein (LFA-1) with ICAM-1, thereby inhibiting T-cell migration and activation on the ocular surface. This directly reduces inflammation.
Secretagogues and Systemic Therapy
For patients with significant systemic dryness (xerostomia and xerophthalmia), medications that stimulate residual gland function are used:
- Secretagogues (Pilocarpine and Cevimeline): These are systemic medications that activate cholinergic receptors, stimulating fluid secretion from the remaining functional lacrimal and salivary gland tissue.
The Strategic Use of Topical Steroids
Topical corticosteroids (steroid drops) are not a long-term solution due to risks of cataract and elevated intraocular pressure, but they are vital for acute symptom control. They are often used as a ‘bridge therapy’ for a short period (2-4 weeks) to rapidly knock down severe inflammation before the slower-acting immunosuppressive drops (Restasis/Xiidra) take full effect.

4. Advanced Interventions and Procedures
When topical drops fail to provide adequate relief, advanced, often office-based, procedures are required to preserve moisture and protect the ocular surface from the destructive forces of Sjögren’s Syndrome and Dry Eye.
Punctal Plugs and Cauterization
These procedures aim to keep existing tears on the ocular surface longer by blocking the drainage system:
- Punctal Plugs: Tiny, biocompatible plugs are temporarily or permanently inserted into the puncta (the small openings in the inner corner of the eyelids) to stop tear drainage into the nasal cavity. This is highly effective, but plugs must be monitored for migration or expulsion.
- Punctal Cauterization: In cases of severe, unresponsive dryness, the puncta may be permanently sealed via thermal or electrical cauterization.
Autologous Serum Tears and Scleral Lenses
These two interventions represent the gold standard for managing the most severe, refractory cases of Sjögren’s Syndrome and Dry Eye:
- Autologous Serum Tears (AST): These are customized drops made from the patient’s own blood plasma, diluted into a tear substitute. AST contains vital growth factors, vitamins, and immune modulators that are essential for corneal epithelial health and healing, and which are entirely absent in standard artificial tears.
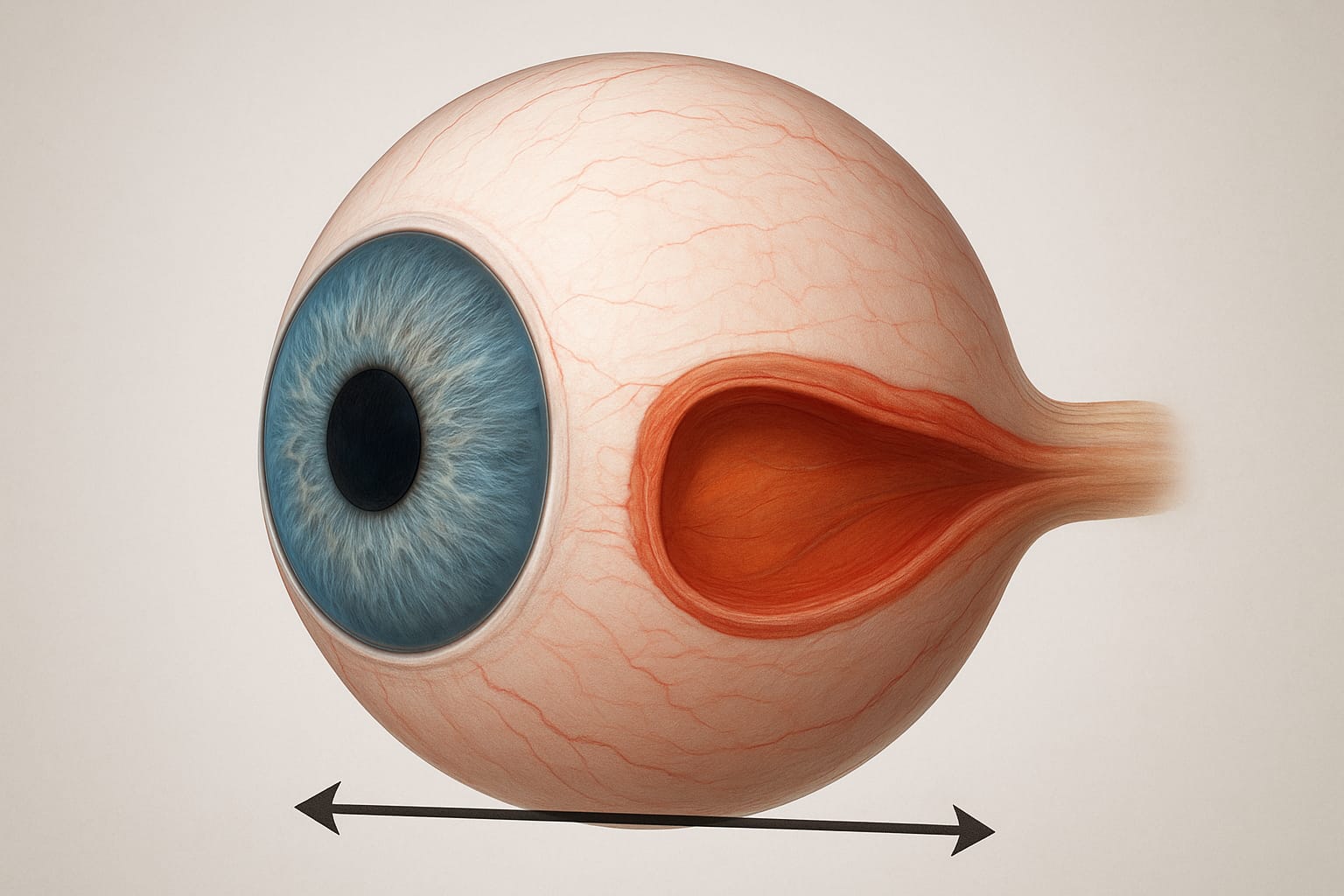
- Scleral Lenses: Large-diameter, gas-permeable contact lenses that rest on the sclera (the white of the eye), vaulting completely over the sensitive cornea. The space between the lens and the cornea is filled with a sterile, non-preserved saline solution, creating a constant, protected, and humid environment. Scleral lenses often provide immediate and dramatic relief from pain and photophobia, acting as a true “liquid bandage” for the severely compromised ocular surface.

Moisture Chamber Glasses
The ultimate relief for severe dry eye. These glasses create a sealed environment to prevent tear evaporation and block painful airflow.
Check Price on Amazon5. Lifestyle, Nutrition, and Supplementation
While systemic medications tackle the immune response, lifestyle changes and targeted nutrition are crucial for maximizing comfort, reducing inflammation, and stabilizing the ocular surface in patients with Sjögren’s Syndrome and Dry Eye.
Omega-3 and Antioxidant Protocols
Chronic inflammation is the root cause of the glandular destruction. Therefore, dietary intervention focuses on potent anti-inflammatories:
- Omega-3 Fatty Acids (EPA/DHA): High-dose supplementation (typically 2000–4000 mg/day) has been shown to improve the quality of the oily layer of the tear film (produced by the Meibomian glands) and reduce the overall systemic inflammatory load.
- Antioxidants (Lactoferrin, Vitamin D): Low levels of Lactoferrin, a protein with antibacterial and anti-inflammatory properties, are common in Sjögren’s tears. Supplemental Vitamin D, which plays a modulatory role in immune function, is also frequently recommended, as deficiency is common in autoimmune patients.
Environmental Control (Humidity and Air Filtration)
Patients with Sjögren’s Syndrome and Dry Eye have minimal tear reserve, making them exquisitely sensitive to dry air and irritants.
- High-Quality Humidifiers: Maintaining bedroom and office humidity levels between 40% and 50% is non-negotiable, particularly during winter or in arid climates.
- Avoidance of Triggers: This includes minimizing exposure to smoke, forced air heating/cooling (aiming diffusers away from the face), and high-altitude travel without specialized eye protection. Wearing wrap-around, moisture-chamber glasses can be vital for outdoor protection.
6. Systemic Management and Coordinated Care
Because Sjögren’s Syndrome affects multiple body systems, successful treatment requires a coordinated, multidisciplinary approach.

Rheumatologist and Ophthalmologist Collaboration
The ophthalmologist is focused on ocular surface preservation, while the rheumatologist manages the overall autoimmune load, fatigue, pain, and systemic complications (such as vasculitis or kidney involvement). Effective communication between these two specialists is paramount to ensure that systemic immunosuppressive therapy (e.g., hydroxychloroquine or methotrexate) complements the topical ocular treatments.
The Link to Fatigue, Pain, and Oral Health
The disease extends far beyond the eyes. The persistent, severe chronic pain and debilitating fatigue are hallmarks of Sjögren’s:
- Pain Management: Neuropathic corneal pain is a common, difficult-to-treat complication requiring specialized attention, often involving oral medications to modulate nerve signals.
- Oral Health (Xerostomia): Severe dry mouth (xerostomia) increases the risk of tooth decay and oral infections. Regular dental visits and specialized oral hygiene products are necessary to manage this aspect of the syndrome, highlighting the need for holistic care.
7. New Horizons in Treatment
Research into Sjögren’s Syndrome and Dry Eye is accelerating, focusing on more specific immunological targets and novel delivery methods.
Biological Therapies and Immunomodulation
The future lies in targeted biologic drugs that modulate specific immune pathways without broadly suppressing the entire system.
- B-Cell Targeted Therapies: Drugs like Rituximab, which target B-cells (responsible for autoantibody production), are being studied extensively to reduce glandular inflammation and improve both ocular and systemic symptoms.
- Infliximab and Anti-TNF Agents: These agents, already used for Rheumatoid Arthritis, are being investigated for their potential to reduce the systemic inflammation driving the syndrome.
Regenerative Medicine and Glandular Repair
Long-term goals include reversing the physical damage to the lacrimal glands:
- Stem Cell Therapy: Research is ongoing into the use of regenerative medicine and stem cells to potentially repair or regenerate the damaged epithelial tissue within the lacrimal glands, offering the hope of restoring natural tear production rather than just managing the deficit.
Frequently Asked Questions (FAQ) about Sjögren’s Syndrome and Dry Eye
- Q: Is Sjögren’s Syndrome contagious?
- A: No. Sjögren’s is an autoimmune disease, meaning it is caused by the body’s own immune system mistakenly attacking healthy tissue. It cannot be caught or transmitted from person to person.
- Q: Does Sjögren’s Syndrome always cause blindness?
- A: No, the disease itself rarely causes blindness. However, the chronic, severe dryness can lead to serious secondary complications like corneal ulcers, infections, and scarring if not aggressively managed. With proper specialist care, vision loss is usually preventable.
- Q: Are artificial tears enough to treat Sjögren’s dry eye?
- A: While artificial tears provide temporary relief, they are generally not sufficient for managing Sjögren’s Syndrome and Dry Eye. Effective treatment requires prescription anti-inflammatory drops (like Restasis or Xiidra), punctual plugs, and often advanced procedures like Autologous Serum Tears or Scleral Lenses to address the underlying inflammation and corneal damage.
- Q: What is the most important vitamin to take for this condition?
- A: Omega-3 fatty acids (specifically EPA and DHA) and Vitamin D are frequently recommended. Omega-3s help reduce systemic inflammation, while Vitamin D plays a crucial role in immune system modulation, which is essential for managing the autoimmune component of the syndrome.
Conclusion: Achieving Stability and Quality of Life
The diagnosis of Sjögren’s Syndrome and Dry Eye marks a transition from routine vision care to advanced, specialized management. This condition requires a paradigm shift—moving past temporary relief to focus on interrupting the autoimmune inflammatory cycle. By leveraging cutting-edge pharmacological agents (immunosuppressive drops), advanced protective strategies (Scleral Lenses, Serum Tears), and proactive systemic coordination between the rheumatologist and ophthalmologist, patients can achieve a significant reduction in pain and a restoration of ocular comfort. While there is no cure, understanding the science of the disease empowers patients to take control of their treatment protocol and maintain a high quality of life and long-term vision health.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."