The preservation of central vision is paramount to maintaining a high quality of life. While standard nutritional advice is a great start, modern AMD Prevention Protocols have evolved into a sophisticated field of neuro-protective science; for a deeper look into the latest clinical breakthroughs, explore our Advanced Vision Therapy & Biohacking Hub. As the leading cause of irreversible vision loss in older adults in developed countries, Age-Related Macular Degeneration (AMD) poses a significant threat to global eye health. However, modern ophthalmology has shifted its focus from merely treating late-stage disease to implementing robust AMD Prevention Protocols. These protocols, backed by decades of rigorous scientific research—most notably the Age-Related Eye Disease Studies (AREDS)—empower individuals to take proactive steps to protect the macula, the small, central area of the retina responsible for detailed, sharp vision.
This definitive guide is designed to serve as your authoritative roadmap. We will delve into the risk factors, the pathology of AMD, and the evidence-based nutritional, pharmacological, and lifestyle strategies that comprise the most effective AMD Prevention Protocols available today. Understanding the difference between dry and wet AMD and knowing which stage requires which protocol is essential for anyone serious about preserving their most precious sense.
1. Understanding AMD: Pathology, Staging, and Risk
Effective AMD Prevention Protocols require a firm understanding of the disease itself—how it develops and the factors that accelerate its progression.
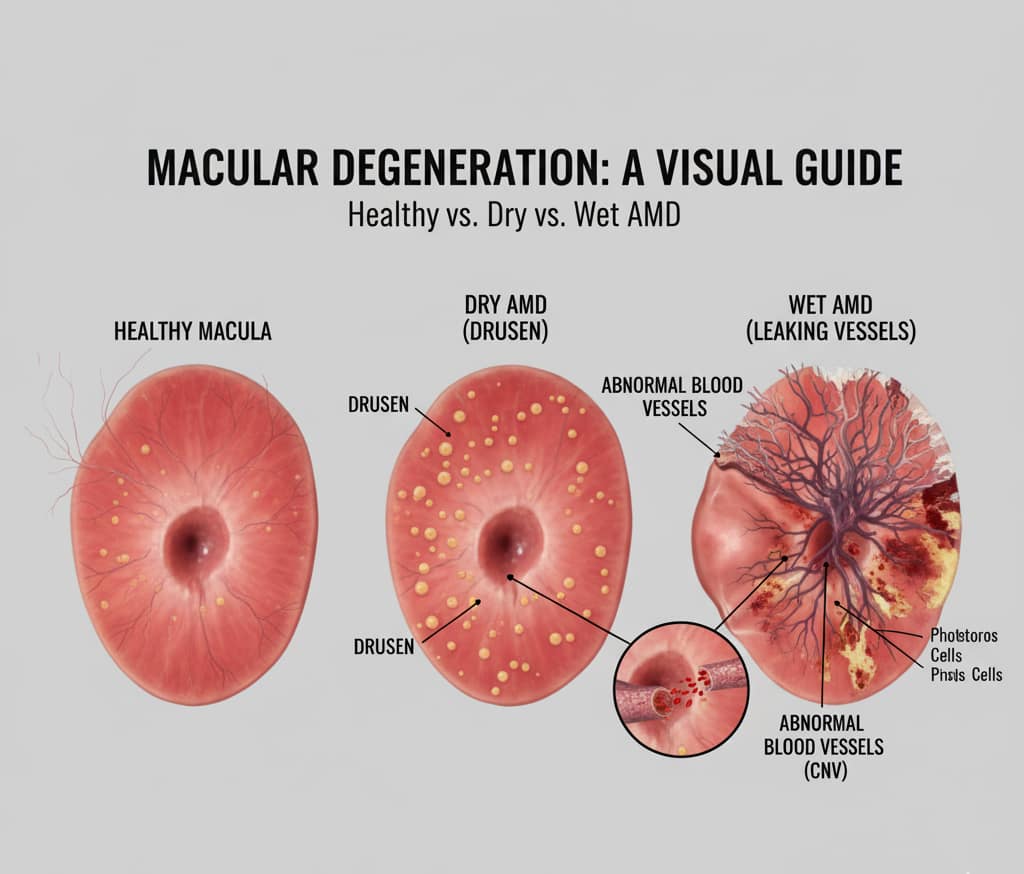
The Two Types of AMD: Dry vs. Wet
- Dry AMD (Atrophic): This is the most common form (80-90% of cases). It is characterized by the gradual breakdown of the light-sensitive cells in the macula. Its hallmark is the presence of drusen—yellow deposits of extracellular material that accumulate beneath the retina. Dry AMD typically progresses slowly.
- Wet AMD (Neovascular/Exudative): Though less common, this form accounts for 90% of severe vision loss associated with AMD. It occurs when abnormal blood vessels (Choroidal Neovascularization, CNV) grow beneath the macula, leaking fluid and blood, causing rapid and severe damage to central vision.
| Feature | Dry AMD (Atrophic) | Wet AMD (Exudative) |
|---|---|---|
| Prevalence | 80-90% of cases | 10-15% of cases |
| Key Sign | Drusen (yellow deposits) | Abnormal blood vessel growth |
| Vision Loss | Slow, gradual blurriness | Rapid, severe distortion |
| Primary Protocol | AREDS 2 & Lifestyle | Anti-VEGF Injections |
Staging: Identifying When to Start Prevention Protocols
Prevention is most effective in the early and intermediate stages, before vision loss is significant.
- Early AMD: Defined by multiple small drusen or a few medium-sized drusen. Often asymptomatic. Prevention Protocols begin here.
- Intermediate AMD: Defined by large drusen or pigmentary changes. Vision may be subtly impaired. This stage requires aggressive, specific AMD Prevention Protocols (e.g., the AREDS formula).
- Advanced AMD (Wet or Geographic Atrophy): Significant central vision loss has occurred. Prevention shifts to management and slowing progression.
Did You Know?
The Age-Related Eye Disease Studies (AREDS) proved that specific high-dose supplementation can reduce the 5-year risk of progression from intermediate to advanced AMD by approximately 25%. This finding established nutritional intervention as the gold standard of **AMD Prevention Protocols** globally.
2. The Cornerstone: AREDS and AREDS 2 Formula
The most robust and scientifically validated AMD Prevention Protocols are built upon the findings of the Age-Related Eye Disease Studies (AREDS and AREDS 2). These studies proved that high-dose nutrient supplementation significantly reduces the risk of moderate to severe vision loss.
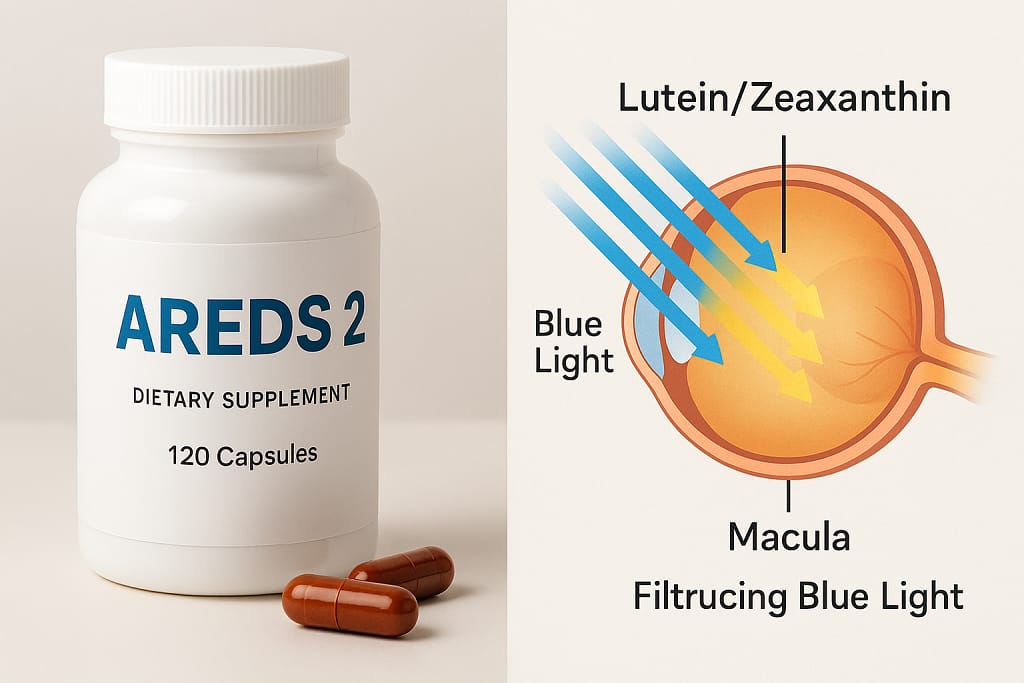
AREDS 2: The Modern Standard of Care
The current standard is the AREDS 2 formulation, which improved upon the original by replacing Beta-carotene (linked to increased risk of lung cancer in smokers) with Lutein and Zeaxanthin. The key components are:
- Vitamin C (Ascorbic Acid): 500 mg
- Vitamin E (dl-alpha tocopheryl acetate): 400 IU
- Zinc (Zinc Oxide): 80 mg
- Copper (Cupric Oxide): 2 mg (added to prevent copper deficiency anemia due to high zinc intake)
- Lutein: 10 mg
- Zeaxanthin: 2 mg
Why Lutein and Zeaxanthin are Biologically Crucial
These two powerful carotenoids form the Macular Pigment—the eye’s internal, biological sun filter. They are the core of the nutritional AMD Prevention Protocols:
- Antioxidant Power: They absorb blue light, acting as a filter and neutralizing harmful free radicals in the macula.
- Macular Pigment Optical Density (MPOD): Low levels of MPOD are a major risk factor for AMD. Supplementation with Lutein and Zeaxanthin has been proven to increase MPOD, physically strengthening the macular tissue against damage.

NOW Foods Lutein & Zeaxanthin
Supports macular health, blue light protection & visual performance.
- 25 mg Lutein + 5 mg Zeaxanthin
- Enhances visual function
- Helps with screen-related eye strain
3. Beyond AREDS 2: Comprehensive Nutritional Protocols
While AREDS 2 is non-negotiable for intermediate AMD, effective AMD Prevention Protocols for all stages extend to overall dietary and supplemental intake.
The Role of Omega-3 Fatty Acids
Omega-3s, particularly Docosahexaenoic Acid (DHA) and Eicosapentaenoic Acid (EPA), are vital components of retinal cell membranes.
- Anti-Inflammatory Action: Omega-3s possess potent anti-inflammatory properties, reducing the chronic inflammation thought to be central to drusen formation and progression from dry to wet AMD.
- Dietary Sources: High consumption of cold-water fatty fish (salmon, mackerel, sardines) twice weekly is highly recommended. Supplementation is often advised, targeting DHA levels found in the retina.
The Significance of Glycemic Load and Diet
Research strongly suggests a link between a high Glycemic Index (GI) diet (rapidly digested carbohydrates) and increased AMD risk.
- Oxidative Stress: High blood sugar fluctuations increase oxidative stress and inflammation, contributing to the formation of drusen and damage to the Retinal Pigment Epithelium (RPE) cells.
- Prevention Strategy: Shifting to a low-GI, Mediterranean-style diet—rich in leafy greens, nuts, fish, and whole grains—is a core part of effective AMD Prevention Protocols.
4. Lifestyle Modulations: External Risk Control
Nutritional protocols address internal defenses, but lifestyle changes are necessary to mitigate external factors that accelerate the disease.
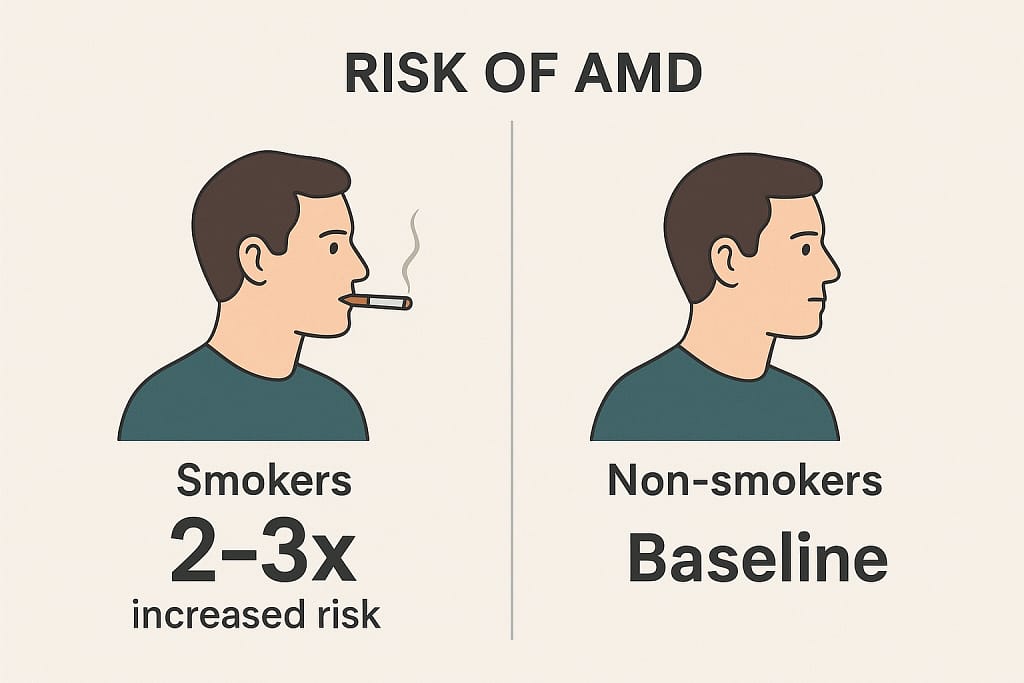
Smoking Cessation: The Single Most Important Step
Smoking is unequivocally the number one modifiable risk factor for AMD. Smokers are up to four times more likely to develop AMD, and they develop it earlier.
- Mechanism of Harm: Smoking reduces the density of the macular pigment, increases oxidative stress, reduces choroidal blood flow, and interferes with the metabolism of essential nutrients like Vitamin C and Zinc.
UV and Blue Light Protection
Chronic exposure to high-energy light accelerates macular damage. This is where protection protocols become a direct extension of AMD Prevention Protocols.
- High-Quality Sunglasses: Sunglasses that block 99-100% of UVA and UVB radiation are essential whenever outdoors.
- Blue Light Management: While Lutein and Zeaxanthin work internally, managing digital blue light exposure and using appropriate computer glasses can reduce potential stress on the RPE cells, particularly important for those already in the early stages of AMD.
5. Pharmacological and Future Interventions
While nutrition and lifestyle form the foundation of AMD Prevention Protocols, the future of macular protection involves targeted medical strategies and emerging regenerative therapies.
Low-Dose Aspirin and Cardiovascular Co-Management
AMD shares several risk factors with cardiovascular disease (CVD), including chronic inflammation and oxidative stress.
- Aspirin Controversy: While low-dose aspirin is common for CVD prevention, its relationship with AMD is complex. Some studies suggest a potential link between daily aspirin use and the development of neovascular (wet) AMD, although results are inconsistent.
- Clinical Protocol: The general consensus for AMD Prevention Protocols is that aspirin should only be continued if clearly indicated for cardiovascular health, and the patient must be closely monitored for signs of wet AMD. Managing co-existing conditions like hypertension and high cholesterol with prescribed medications is a necessary complementary protocol.
Emerging Therapies: Anti-VEGF for Dry AMD and Genetic Research
The biggest breakthroughs in AMD treatment are shifting towards intervening in the early, dry stages of the disease.
- Complement System Inhibitors: A major driver of drusen formation is chronic, uncontrolled activity in the immune system’s complement cascade. New drugs are being developed to inhibit components of this system (e.g., C3 and C5 inhibitors) to prevent the inflammatory process that leads to RPE cell death (Geographic Atrophy).
- Gene Therapy and Regeneration: The long-term future of AMD Prevention Protocols may involve gene therapy to protect RPE cells from damage or to regenerate photoreceptor cells lost to the disease. This research promises to eventually move beyond mere slowing of progression to potential restoration of function.
Quick Check: Are You Following AMD Protocols?
Next Step: If you checked 2 or more boxes, you should initiate professional AMD Prevention Protocols and schedule a dilated eye exam immediately.
6. Monitoring and Clinical Biometrics
The most effective AMD Prevention Protocols are useless without consistent monitoring. Early detection of conversion from dry to wet AMD is vital for saving central vision.
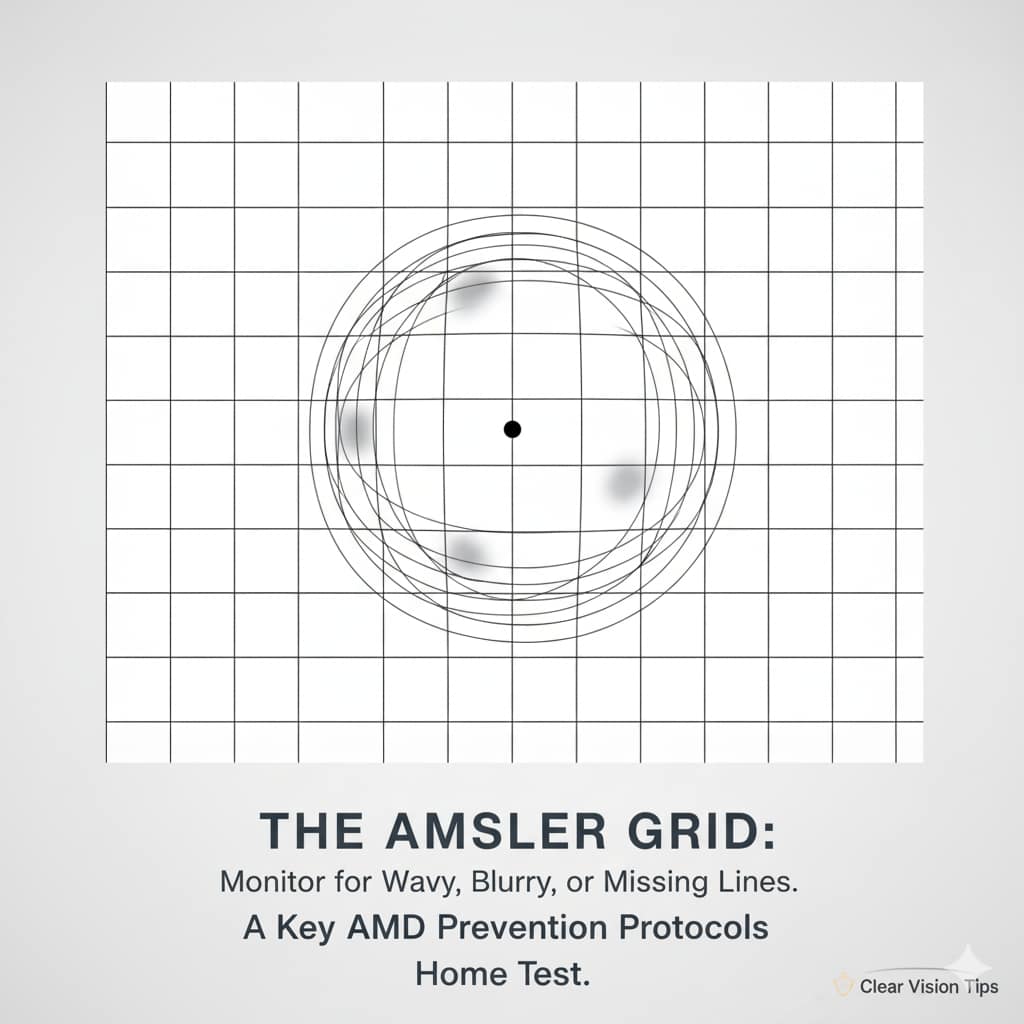
The Amsler Grid: Daily Monitoring at Home
The Amsler Grid is a simple but critical diagnostic tool for patients with intermediate or advanced AMD, designed for daily self-testing.
- Purpose: It detects subtle changes in central vision, specifically metamorphopsia (distortion of straight lines) or scotoma (a blind spot), which are often the first signs of fluid leakage or CNV growth associated with wet AMD.
- Protocol: Patients should check each eye separately, daily. Any sudden change, waviness, or missing areas must prompt an immediate call to the retina specialist.
Measuring Macular Pigment Optical Density (MPOD)
MPOD measurement is the only objective biomarker that quantifies the protective layer of Lutein and Zeaxanthin in the macula.
- Biometric Feedback: Many clinicians use MPOD devices to measure pigment density. This allows for personalized titration of nutritional AMD Prevention Protocols—ensuring the patient is actually absorbing and utilizing the protective carotenoids effectively.
Genetic Testing: Identifying High-Risk Individuals
Certain gene variants are known to significantly increase the risk of AMD, particularly variants in the Complement Factor H (CFH) gene.
- Proactive Screening: Genetic testing allows ophthalmologists to identify individuals with the highest lifetime risk, allowing them to initiate aggressive AMD Prevention Protocols (smoking cessation, rigid adherence to AREDS 2, and specialized dietary changes) much earlier, before the disease becomes clinically evident.
7. Holistic Protocols for Reducing Oxidative Stress
AMD is fundamentally an oxidative and inflammatory disease. Holistic protocols target systemic health to reduce the overall biological burden on the fragile macular tissue.
Exercise and Ocular Blood Flow
Regular physical activity is an underestimated component of AMD Prevention Protocols.
- Mechanism: Aerobic exercise improves systemic circulation, which enhances oxygen and nutrient delivery to the choroid and RPE cells. Better blood flow helps remove metabolic waste (which contributes to drusen) more efficiently.
- Protocol: Aim for at least 150 minutes of moderate aerobic activity per week, maintaining a healthy weight to reduce chronic systemic inflammation.
Stress Management and the Inflammation Link
Chronic psychological stress elevates cortisol levels, which fuels persistent, low-grade inflammation throughout the body—including the eye.
- The Cytokine Cascade: Stress can accelerate the release of pro-inflammatory cytokines, potentially worsening the underlying conditions that lead to AMD progression.
- Holistic Strategy: Techniques such as mindfulness meditation, yoga, and ensuring adequate sleep are necessary adjuncts to clinical protocols to suppress systemic inflammation.
Vitamin D and Immune Modulation
Vitamin D is crucial for immune function and is believed to play a role in modulating inflammation, a primary mechanism in AMD pathology.
- Research Link: Low Vitamin D levels have been associated with increased risk of AMD onset and progression.
- Prevention Protocol: While research is ongoing, ensuring adequate Vitamin D levels (often through supplementation, especially in northern climates) is a sensible addition to the nutritional pillars of AMD Prevention Protocols.
Frequently Asked Questions (FAQ) about AMD Prevention Protocols
Q: Who should take the AREDS 2 supplements? A: The AREDS 2 formula is specifically recommended for individuals diagnosed with Intermediate AMD or Advanced AMD in one eye. There is no proven benefit for individuals with early AMD or those with no signs of the disease.
Q: Can a healthy diet replace AREDS 2 supplements? A: For those with Intermediate AMD, a healthy diet alone is usually not enough to provide the high, therapeutic doses of vitamins and minerals proven to slow progression (e.g., 10 mg Lutein). Diet should complement the AREDS 2 supplement, not replace it.
Q: How does smoking affect my AMD risk? A: Smoking is the single largest modifiable risk factor. It not only increases your risk of developing AMD by up to four times but also interferes with the absorption and effectiveness of the protective nutrients, effectively undermining all AMD Prevention Protocols.
Q: How long do I need to take the AREDS 2 formula? A: Supplementation is recommended to be taken indefinitely (for life) to continue receiving the protective benefits and to slow the rate of progression of AMD.
Conclusion: The Power of Proactive Macular Care
Age-Related Macular Degeneration is a chronic, progressive disease, but it is no longer an inevitable consequence of aging. The definitive AMD Prevention Protocols are a powerful combination of clinical science and empowered self-care. By rigidly adhering to the AREDS 2 nutritional blueprint, eliminating smoking, adopting a low-glycemic, anti-inflammatory diet, and diligently utilizing home monitoring tools like the Amsler Grid, individuals can significantly alter their trajectory. The future of vision health lies in prevention, offering a concrete path to preserve the quality of life dependent on sharp, central vision.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."