Understanding Medication Side Effects Eyes is a vital part of modern healthcare. Many of us take prescriptions for blood pressure, inflammation, or allergies without realizing they can quietly impact our sight. Because eye tissue is so delicate, certain chemicals can cross the Blood-Retinal Barrier and accumulate where they don’t belong, leading to permanent damage if left unmonitored.
Important Note: Managing Medication Side Effects Eyes requires a deep understanding of your overall health. If you are noticing changes in your vision while on a new prescription, visit our Eye Symptoms & Relief HUB to find specific diagnostic protocols.
1. How Do Drugs Actually Damage Your Sight?
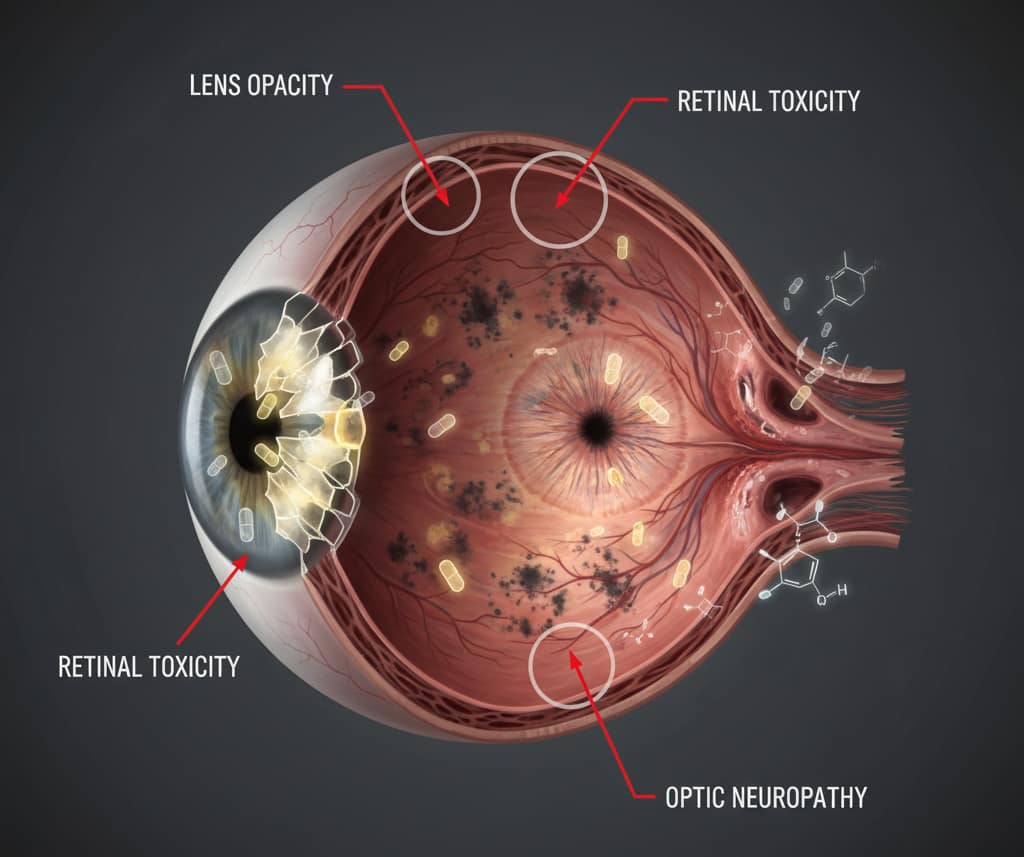
Instead of complex pharmacology, think of your eye as a high-precision filter. Some medications are “lipophilic” (fat-soluble), meaning they easily slip past the eye’s natural defenses. Once inside, they typically cause damage in three ways:
- Lens Clouding: Leading to drug-induced cataracts.
- Optic Nerve Damage: Cutting off the communication between your eye and brain.
- Retinal Toxicity: Destroying the cells responsible for your central vision.
2. High-Risk Prescriptions: Common Medication Side Effects Eyes
This section covers the “Heavy Hitters” that require mandatory eye monitoring.
Antimalarials (Plaquenil/Hydroxychloroquine)
Used widely for Lupus and Rheumatoid Arthritis, Plaquenil can deposit in the retina over years. This causes “Bull’s Eye Maculopathy,” a permanent loss of central vision. The American Academy of Ophthalmology mandates annual screenings after 5 years of use to catch damage before symptoms appear.
Corticosteroids (Prednisone, Dexamethasone)
Whether taken as pills, inhalers, or eye drops, steroids are “silent thieves.” They can spike your intraocular pressure (IOP), leading to Steroid-Induced Glaucoma or specialized cataracts.
ED Medications (Viagra, Cialis)
These drugs can cause a transient “blue tinge” to your vision. In rare but serious cases, they are linked to NAION—a sudden, painless loss of vision caused by reduced blood flow to the optic nerve.
Did You Know?
The risk of Hydroxychloroquine (Plaquenil) toxicity rises sharply after 5 years of use, specifically when the cumulative dose exceeds 1,000 grams. Once vision loss occurs due to Plaquenil retinopathy, it is often irreversible, making annual screening tests (OCT and Visual Fields) mandatory for long-term users, even if they show no symptoms.
3. Symptom Tracker: When to Call Your Doctor
Use this table to identify which Medication Side Effects Eyes match your current prescription.
| Drug Class | Potential Eye Symptom | Urgency Level |
| Corticosteroids | Blurred vision, halos around lights | Moderate |
| Antimalarials | Missing spots in central vision | High (Mandatory) |
| Antihistamines | Grittiness, severe dryness, redness | Low |
| ED Medications | Blue-tinted vision, sudden vision loss | EMERGENCY |

4. Protecting Your Vision (The Biohacking Approach)
If you must stay on a high-risk medication, you can support your ocular health through targeted nutrition:
- Omega-3 Fatty Acids: Critical for fighting drug-induced dry eye and inflammation.
- Lutein & Zeaxanthin: These antioxidants act as internal “sunglasses” for your retina.
- Hydration: Essential if you take decongestants or diuretics which strip moisture from the eyes.

Preservative-Free Relief Drops
Perfect for neutralizing Medication Side Effects Eyes like chronic grittiness and dryness caused by antihistamines.
❓ Frequently Asked Questions (FAQ)
Can common prescriptions cause permanent vision loss?
Answer: Yes, certain Medication Side Effects Eyes can lead to irreversible damage if not caught early. High-risk drugs like Hydroxychloroquine (Plaquenil) can cause permanent retinal toxicity, while long-term steroid use may lead to blindness via induced glaucoma. Baseline exams are essential for prevention.
How do I know if my blurry vision is one of the Medication Side Effects Eyes?
Answer: If you notice sudden blurring, halos around lights, or changes in color perception shortly after starting a new prescription, these are likely Medication Side Effects Eyes. You should consult an ophthalmologist immediately to distinguish between simple dry eye and serious drug-induced ocular toxicity.
Which drug classes are most notorious for Medication Side Effects Eyes?
Answer: The most frequent culprits for Medication Side Effects Eyes include systemic corticosteroids, antimalarials, certain cardiovascular drugs (like Amiodarone), and even over-the-counter antihistamines. Each class affects different parts of the eye, from the cornea to the optic nerve.
Are Medication Side Effects Eyes reversible once you stop the drug?
Answer: Reversibility depends on the specific drug and the type of damage. While Medication Side Effects Eyes like corneal deposits or steroid-induced pressure spikes may resolve after stopping the medication, retinal scarring or optic nerve atrophy are typically permanent.
Can over-the-counter allergy meds cause Medication Side Effects Eyes?
Answer: Absolutely. Many people don’t realize that chronic dry eye is one of the most common Medication Side Effects Eyes caused by OTC antihistamines and decongestants. These drugs reduce tear production, leading to persistent irritation and potential corneal micro-scratches.
Conclusion: Collaborative Care for Lifelong Vision Health
While the risk of ocular drug toxicity is a serious concern in modern medicine, it is a manageable risk when approached with proactive awareness. Protecting your sight does not mean avoiding necessary systemic treatments; rather, it requires a collaborative care model where your prescribing physician and your ophthalmologist work in perfect sync to monitor your health.
By establishing a clear baseline and staying vigilant for early warning signs, you can benefit from life-saving medications without sacrificing your vision. Your eyes are often the first place where systemic changes manifest, making them a vital “early warning system” for your overall well-being. Do not wait for symptoms to appear, as some changes can be silent and irreversible.
Call to Action: If you are starting a new high-risk medication or have been on a long-term prescription without a recent check-up, consult your eye doctor immediately to schedule a comprehensive exam. Taking this single step today is the best investment you can make for a lifetime of clear vision.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."



