Chronic dry eye disease is far more complex than a simple lack of tears. For millions of sufferers, the root cause lies not in insufficient water production, but in the failure of the oil-producing glands of the eyelids: the Meibomian Glands. This condition, known as Meibomian Gland Dysfunction (MGD), is the single most common cause of evaporative dry eye and is inextricably linked to chronic Blepharitis—an inflammatory condition of the eyelids.
Ignoring MGD leads to a cycle of discomfort, redness, and potential damage to the ocular surface. However, modern ophthalmology has moved beyond symptomatic treatment, developing comprehensive, multi-faceted MGD Protocol strategies designed to restore glandular function, stabilize the tear film, and provide lasting relief.
This definitive guide breaks down the science behind MGD and Blepharitis, presenting the essential 3-Step Home Care Protocol, the most effective advanced medical interventions, and the nutritional and lifestyle biohacks necessary to finally reclaim ocular comfort.
Recent clinical data from the National Institutes of Health (NIH) suggests that up to 86% of all dry eye patients suffer from some form of Meibomian Gland Dysfunction.
1. Understanding MGD and Blepharitis: The Anatomy of Ocular Discomfort
Before implementing the MGD Protocol, it is vital to understand the delicate anatomy of the tear film and the pathology of the glands.
The Tear Film: A Three-Layered Defense
The tear film is not just water; it is a three-layered structure that lubricates, protects, and nourishes the eye:
- Mucin Layer: The innermost layer, produced by goblet cells, allows the tear film to adhere to the cornea.
- Aqueous (Water) Layer: The middle and thickest layer, produced by the lacrimal glands.
- Lipid (Oil) Layer: The outermost layer, produced by the Meibomian Glands, which prevents the aqueous layer from evaporating too quickly.
Meibomian Gland Dysfunction (MGD): The Problem of the Oil Layer
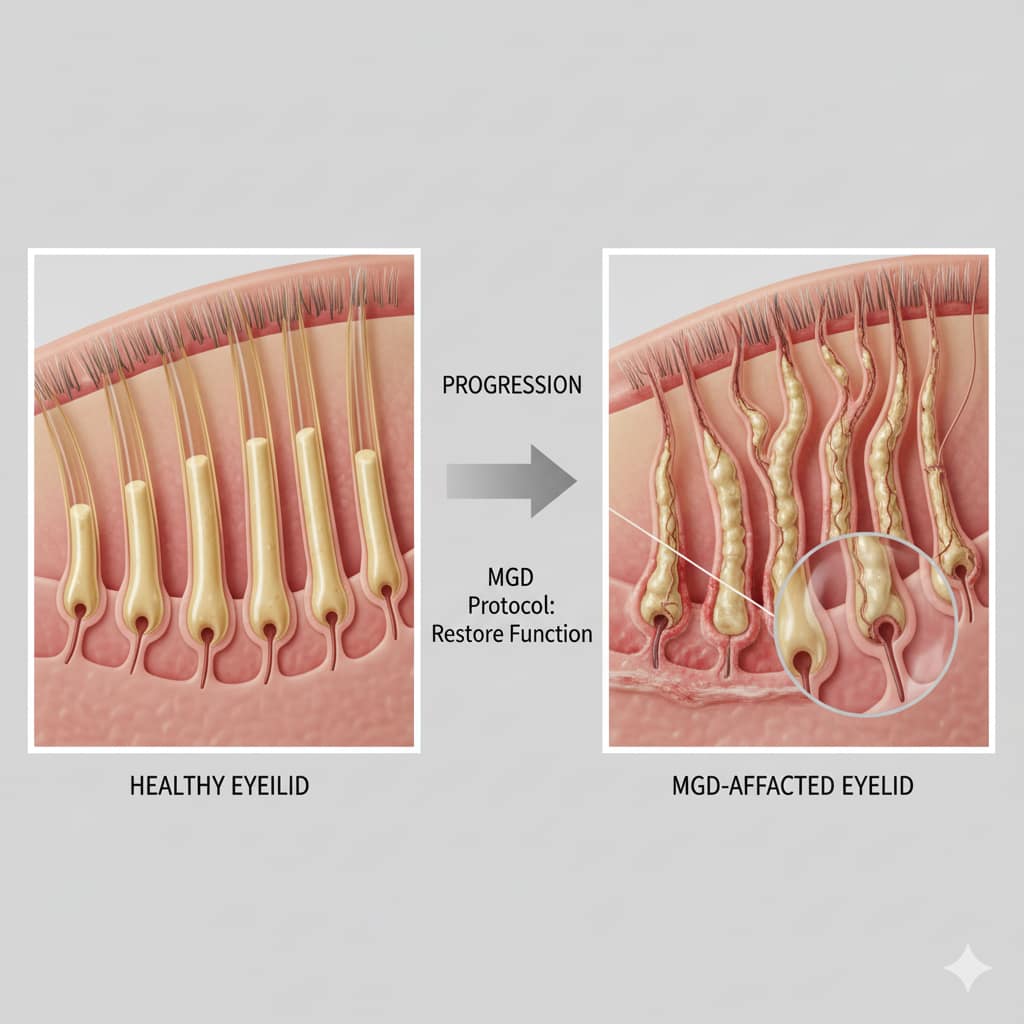
MGD occurs when the Meibomian Glands—located vertically within the upper and lower eyelids—become blocked or their oil (meibum) becomes thick and viscous.
- Pathology: The glands produce an insufficient quantity or poor quality of meibum. Without a healthy lipid layer, the watery tears evaporate rapidly, leading to the characteristic burning, grittiness, and redness of evaporative dry eye.
- Consequence: Blockage leads to gland atrophy (shortening and scarring of the glands), making the condition irreversible if not treated aggressively and early.
Blepharitis: The Inflammatory Component
Blepharitis is the inflammation of the eyelids, which often co-exists with MGD and creates a vicious cycle of irritation.
- Anterior Blepharitis: Affects the outer front surface of the eyelid, often caused by bacteria (Staphylococcus) or mites (Demodex).
- Posterior Blepharitis (MGD): Affects the inner part of the eyelid where the Meibomian Glands open. MGD is essentially a form of posterior blepharitis.
2. The Core 3-Step MGD Protocol: Home Care Essentials
The foundation of every successful MGD Protocol lies in consistent, daily home care designed to liquefy the clogged oil (meibum), express the glands, and clean the eyelid margin.
Step 1: Thermal Therapy (Warming)
Heat is the crucial first step. Meibum solidifies at body temperature; applying heat melts the blockage.
- Method: Use a specialized, consistent heat source (e.g., heated eye mask, often powered by USB or microwave) designed to maintain a temperature between 40-45°C (104-113°F).
- Protocol: Apply the mask for 10-15 minutes, twice daily. The heat must be consistent and sustained throughout the duration to be effective. Avoid using a hot washcloth; it cools too quickly and is inefficient.

Professional USB Heated Eye Mask
Unlike washcloths, this mask maintains a steady 113°F for 15 minutes—the exact temperature needed to melt blocked meibum.
Check Price on AmazonStep 2: Mechanical Therapy (Expression/Massage)
Immediately after heating, the liquefied meibum must be expressed from the glands.
- Method: Gently massage the eyelids. Use a clean fingertip or cotton swab to roll or press along the eyelids from top to bottom (upper lid) and bottom to top (lower lid), applying mild pressure towards the lash line.
- Protocol: Perform the massage for 30 seconds per eyelid, immediately after removing the mask. This step is often overlooked but is essential for preventing the re-clogging of the glands.
Step 3: Hygiene Therapy (Cleaning)
Cleaning removes the debris, bacteria, and biofilm that accumulate on the eyelid margin, preventing blockages from reforming.
- Method: Use a specialized eyelid cleanser (e.g., hypochlorous acid spray or commercially prepared lid wipes).
- Protocol: Gently scrub the base of the eyelashes and the lid margin for 30 seconds, once daily, typically in the morning or evening. This step manages the Blepharitis component of the disease.

Hypochlorous Acid Eyelid Spray
Eliminates 99.9% of bacteria and Demodex mites that cause Blepharitis. Gentle, non-irritating, and highly effective.
View on Amazon →Did You Know?
It is estimated that over 86% of dry eye cases involve Meibomian Gland Dysfunction (MGD). This means that focusing solely on water-based eye drops without addressing the underlying oil deficiency (meibum) will fail to provide long-term relief. The 3-Step **MGD Protocol** is essential because it targets the root cause.
3. Advanced Topical Biohacking: Prescription and OTC Solutions
For moderate to severe MGD, home therapy must be supported by targeted prescription or specialized over-the-counter (OTC) topical agents.
Demodex Protocol: Targeting Eyelid Mites
Demodex mites are microscopic organisms that live at the base of the eyelashes and are frequently implicated in chronic blepharitis and MGD.
- Symptoms: Waxy, cylindrical dandruff (sleeves) at the base of the lashes, often worse in the morning.
- Protocol: Use Tea Tree Oil (TTO) based cleansers (diluted for safety) or, more effectively, prescription Lotilaner ophthalmic solution (e.g., XDEMVY). TTO is a powerful biohack, but Lotilaner provides targeted, long-term mite eradication, relieving the inflammation they cause.
Topical Antibiotics and Anti-Inflammatories
Chronic MGD often involves a change in the bacterial flora and uncontrolled inflammation.
- Low-Dose Topical Azithromycin: Used for its anti-inflammatory properties and its ability to modulate the Meibomian Glands themselves, not just for its antibiotic effect. It changes the composition of the oil.
- Topical Corticosteroids (Short Term): Used briefly (e.g., 2-4 weeks) to “break the cycle” of severe inflammation and allow the other MGD protocols to take effect. Must be used under ophthalmological supervision due to risk of increased eye pressure.

Ocular Surface Immunomodulation
Cyclosporine and Lifitegrast are drops that target the underlying immune-mediated inflammation that damages the tear-producing glands.
- Mechanism: These drops suppress the activity of inflammatory cells (T-cells) on the ocular surface, allowing the lacrimal and Meibomian Glands to function more normally. They are essential for long-term stabilization in persistent MGD/Dry Eye.
4. In-Office MGD Treatments: When Home Care Isn’t Enough
When home care and topical drops fail to restore gland function (often due to advanced gland blockage or atrophy), in-office procedures provide a powerful therapeutic intervention.
Thermal Pulsation Devices
This is the gold standard for many chronic MGD sufferers.
- Mechanism (Example: LipiFlow): The device applies controlled, therapeutic heat (42.5°C) directly to the inner eyelid surfaces while simultaneously providing pulsating pressure to gently “milk” or express the solidified meibum from the glands.
- Benefit: Provides a highly effective, sustained treatment that is significantly more efficient than manual home expression.
Intense Pulsed Light (IPL) Therapy
IPL, originally used in dermatology, has proven highly effective for MGD, particularly when associated with Rosacea (which frequently affects the eyes).
- Mechanism: Flashes of intense light are applied to the skin around the eyelids. This heat seals abnormal blood vessels (telangiectasias) that release inflammatory mediators into the meibomian glands. It also kills Demodex mites and melts deep blockages.
- Protocol: Typically requires a series of 3-4 treatments, 3-4 weeks apart, followed by maintenance treatments.
⚠️ Avoid the “Washcloth Trap”
A wet washcloth loses its therapeutic heat in less than 2 minutes. To melt the thick oils inside your glands, you need sustained heat for at least 10 minutes. This is why a dedicated eye mask is the only way to truly follow the MGD Protocol effectively.
Manual Gland Expression and Microblepharoexfoliation
- Manual Expression: The doctor uses specialized forceps to physically squeeze or express meibum from severely clogged glands after topical anesthetic and heating.
- Microblepharoexfoliation (Example: BlephEx/AB Max): A rotary medical sponge is used to gently and precisely exfoliate the eyelid margin, removing the biofilm, debris, and stubborn mite eggs that home cleaning cannot touch. This jumpstarts the hygiene part of the MGD Protocol.
5. Nutritional Protocols: Systemic Support for Gland Function
The quality of the meibum—the oil itself—is directly influenced by systemic factors, making nutrition a critical component of any comprehensive MGD Protocol.
Omega-3 Fatty Acids: The Lipid Layer Modulator
Omega-3s, particularly the EPA and DHA components, are the primary systemic biohack for MGD.
- Mechanism: These healthy fats are incorporated into the meibum, helping to reduce its viscosity (making it thinner and easier to flow) and simultaneously reducing chronic systemic inflammation.
- Protocol: Aim for a high-quality, high-potency fish oil supplement providing at least 1,000 to 2,000 mg of combined EPA + DHA daily. The ratio of Omega-3 to Omega-6 is also important.
Antioxidants: Vitamins A, C, and E
These vitamins support the health of the epithelial cells lining the glands and protect against oxidative damage.
- Vitamin A: Essential for the health and regeneration of the epithelial surface (skin and mucous membranes) of the eyelids and conjunctiva.
- Vitamin C and E: Powerful antioxidants that protect the delicate oils in the glands from becoming rancid or chemically damaged by inflammation.

Water Intake and Electrolyte Balance
While MGD is an oil deficiency, chronic dehydration worsens the aqueous component of the tears, creating a greater dependence on the fragile lipid layer.
- Protocol: Maintain optimal hydration. For some, adding quality electrolytes (sodium, potassium, magnesium) can improve cellular hydration and overall ocular comfort.
6. Lifestyle Modulations and Recurrence Prevention
MGD is a chronic, relapsing condition. Long-term success of the MGD Protocol depends entirely on consistent lifestyle adherence and eliminating common irritants.
Environmental Stress Management
- Air Flow Avoidance: Avoid direct exposure to forced air (car vents, hair dryers, fans). This accelerates evaporation and dries out the eyes, stressing the MGD.
- Screen Time Protocol (20-20-20 Rule): Digital screens drastically reduce blink rate, leading to poor meibum expression. Implement the 20-20-20 rule (every 20 minutes, look 20 feet away for 20 seconds) to force blinking and restore tear film stability.
The Make-Up Biohack: Clean Eyelid Margins
- Avoid Eyeliner and Mascara: Products applied near the inner lid margin (waterline) directly block the Meibomian Gland openings, which is the primary driver of MGD.
- Rigorous Removal: Always ensure 100% removal of all makeup daily using gentle, oil-free cleansers to prevent residue buildup on the lash line.
Chronic Condition Co-Management
Conditions like Rosacea, Thyroid disease, and certain medications (e.g., antihistamines, some acne treatments, and hormone replacement therapies) can severely impact MGD.
- Protocol: Work closely with your primary care physician and ophthalmologist to manage underlying systemic conditions and adjust medications that contribute to glandular dysfunction.
MGD is the primary reason many people wake up with sticky or gritty eyes. If this is your main symptom, consult our guide on Dry Eyes in the Morning to see how to adjust your nighttime routine.
Frequently Asked Questions (FAQ) about MGD Protocols
Q: Is MGD curable? A: MGD is a chronic, manageable condition, but it is not typically curable if gland atrophy has already occurred. The MGD Protocol is designed to control symptoms, restore function, and prevent further atrophy, often requiring lifelong maintenance.
Q: How quickly will I see results from the 3-Step Home Protocol? A: Most patients notice significant symptom improvement (reduced grittiness, redness) within 2 to 4 weeks of rigorous, twice-daily adherence to the heat, expression, and hygiene steps.
Q: What is the most common reason the MGD Protocol fails? A: Failure is almost always due to lack of consistency or ineffective heat. The home protocol must be done consistently, and the heat must be sustained (10+ minutes at >40°C) to effectively melt the meibum.
Q: Can I stop Omega-3 supplements once my eyes feel better? A: It is strongly advised to maintain Omega-3 supplementation. Stopping them can lead to the meibum oil becoming thicker and more inflammatory again, causing a recurrence of MGD symptoms.
Conclusion: Making the MGD Protocol a Lifestyle
Meibomian Gland Dysfunction and chronic Blepharitis demand respect and daily attention. By implementing the robust, evidence-based MGD Protocol—combining targeted thermal and hygiene therapy, advanced topical agents, and systemic nutritional support—you are actively biohacking your ocular comfort. This commitment moves you from merely managing irritating symptoms to restoring the foundational health of your tear film, ensuring clear, comfortable vision for years to come.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."