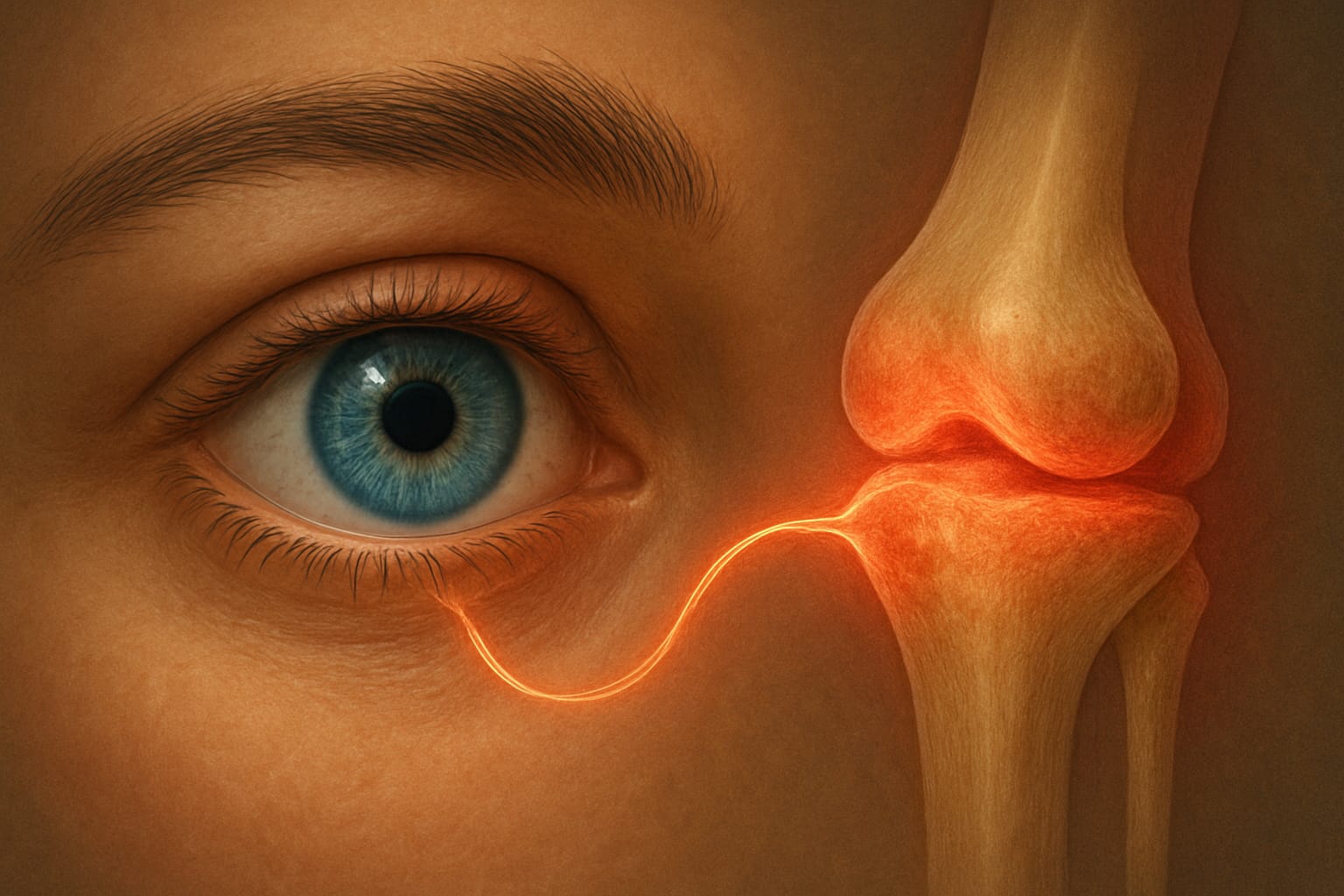
Before diving into specific complications: It is essential to understand the foundation of modern ocular treatments. Check out our comprehensive guide on Eye Conditions & Treatments: Advanced Medical & Natural Solutions to see how RA-related issues fit into the broader spectrum of eye care. Rheumatoid Arthritis (RA) is far more than a condition affecting the joints; it is a chronic, systemic autoimmune disease that can impact virtually any organ system in the body, including the eyes. For millions living with RA, ocular involvement is a significant, yet often overlooked, aspect of their disease. The immune system, mistakenly attacking the body’s own tissues, can lead to a spectrum of Rheumatoid Arthritis Eye Complications, ranging from irritating dry eye to sight-threatening inflammation.
Understanding the profound link between RA and eye health is crucial for early detection, effective management, and vision preservation. This definitive guide delves into the intricate mechanisms by which RA affects ocular tissues, details the specific eye complications—including the severe risks of scleritis and uveitis, and the widespread impact of keratoconjunctivitis sicca (dry eye)—and outlines advanced diagnostic and treatment protocols. We will also explore the critical role of interdisciplinary care and vision biohacking strategies to empower individuals with RA to proactively protect their precious eyesight.
1. The Systemic-Ocular Link: Understanding How RA Impacts Vision
Rheumatoid Arthritis creates an environment of chronic systemic inflammation, driven by an overactive immune response. This section explains how this inflammation translates into Rheumatoid Arthritis Eye Complications.
Autoimmunity and Ocular Inflammation
- Detail the pathophysiology: how inflammatory cytokines (e.g., TNF-alpha, IL-6) and autoantibodies (rheumatoid factor, anti-CCP) circulate throughout the body and can target ocular tissues. Explain the concept of immune privilege in the eye and how it can be compromised in systemic autoimmune diseases. Discuss how the same immune cells that attack joints can infiltrate the sclera, uvea, and lacrimal glands.
Secondary Sjögren’s Syndrome in RA Patients
- Explain the strong association between RA and secondary Sjögren’s Syndrome, where the immune system specifically attacks moisture-producing glands (lacrimal and salivary). Detail how this dramatically contributes to severe dry eye, a primary Rheumatoid Arthritis Eye Complication.
2. The Most Serious Eye Complications of Rheumatoid Arthritis
While dry eye is common, certain Rheumatoid Arthritis Eye Complications represent ocular emergencies that can lead to permanent vision loss if not addressed promptly.
Scleritis and Episcleritis (The Eye Wall)
- Episcleritis: Describe it as a benign, self-limiting inflammation of the superficial sclera.
- Scleritis: Emphasize this as a severe, painful, and often necrotizing inflammation of the deeper sclera. Discuss different types (diffuse, nodular, necrotizing) and the critical difference in pain (deep, boring pain radiating to the jaw/temple). Detail the risk of scleral thinning and perforation.
- Emergency Status: Explain why scleritis is an ocular emergency, often indicative of poorly controlled systemic RA activity.
Uveitis (Internal Inflammation)
- Anterior Uveitis: Inflammation of the iris and ciliary body (iritis). Symptoms: pain, redness (ciliary flush), photophobia, decreased vision.
- Posterior Uveitis/Panuveitis: Inflammation of the retina and choroid. More subtle symptoms but higher risk of permanent vision loss.
- Mechanism in RA: Discuss how immune complexes and inflammatory cells can damage the uveal tract.
Peripheral Ulcerative Keratitis (PUK)
- Describe this rare but devastating complication: severe, crescent-shaped corneal ulceration, often associated with necrotizing scleritis. Emphasize the rapid progression and high risk of corneal perforation, leading to severe vision loss or even globe rupture. This is a true ocular emergency.
Did You Know?
Scleritis, the severe inflammation of the white outer layer of the eyeball (sclera), is often the first and most painful symptom of active Rheumatoid Arthritis (RA). Unlike common eye redness, scleritis is typically an ocular emergency requiring high-dose systemic therapy, as it can be associated with tissue-melting diseases like Peripheral Ulcerative Keratitis (PUK).
3. Keratoconjunctivitis Sicca (Severe Dry Eye): The Most Common RA Complication
While less dramatic than scleritis, chronic severe dry eye is arguably the most prevalent and debilitating Rheumatoid Arthritis Eye Complication, significantly impacting quality of life. Because RA often destroys the moisture-producing glands, many patients suffer from a severe form of evaporative dry eye. For a step-by-step approach to restoring these glands, see our Definitive MGD Protocol: A 3-Step Guide to Conquering Chronic Dry Eye.
Why Dry Eye is Worse with RA (Secondary Sjögren’s)
- Elaborate on the mechanism of secondary Sjögren’s Syndrome: autoimmune destruction of the lacrimal glands, leading to inadequate aqueous tear production. Explain the inflammatory cycle on the ocular surface exacerbated by RA. Discuss the impact on corneal health and visual clarity.
Advanced MGD and Inflammation Management in RA Patients
- Connect RA-related dry eye to Meibomian Gland Dysfunction (MGD), which is often exacerbated by systemic inflammation. Discuss how chronic inflammation can damage meibomian glands. Detail advanced management strategies:
- LipiFlow/IPL for MGD.
- Prescription drops (Cyclosporine, Lifitegrast) for underlying inflammation.
- Autologous serum tears for severe cases.

4. Advanced Treatment Protocols for RA-Related Eye Disease
Managing Rheumatoid Arthritis Eye Complications requires a multi-faceted approach, often involving systemic and topical therapies.
Systemic Immunosuppression (Biologics and DMARDs)
The use of advanced biologics has revolutionized the management of systemic inflammation, as detailed in the clinical guidelines by the American College of Rheumatology, which emphasizes the importance of early aggressive therapy to prevent organ damage, including ocular complications.
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs): Methotrexate, Sulfasalazine, etc. Explain how these drugs control systemic inflammation, which in turn reduces ocular manifestations.
- Biologics: Anti-TNF agents (e.g., Adalimumab, Etanercept), Rituximab. Discuss their targeted action on inflammatory pathways and their efficacy in severe ocular RA (scleritis, PUK, uveitis). Emphasize the importance of tight control of systemic RA for ocular health.
Topical Anti-Inflammatory Agents (Corticosteroids, Cyclosporine, Lifitegrast)
- Detail the role of topical steroids (short-term for acute flares), topical Cyclosporine (Restasis/Cequa) and Lifitegrast (Xiidra) for long-term management of ocular surface inflammation and tear production.
Surgical Interventions (When Necessary)
- Briefly mention surgical options for complications: corneal transplants for severe PUK, glaucoma surgery for steroid-induced glaucoma.

5. Vision Biohacking and Lifestyle Management for RA Patients
Beyond medical treatments, integrating lifestyle modifications and nutritional strategies can significantly support ocular health in RA.
Diet and Anti-Inflammatory Supplements (Omega-3s, Curcumin)
- Anti-Inflammatory Diet: Discuss the benefits of a Mediterranean-style diet (rich in fruits, vegetables, healthy fats) to reduce systemic inflammation.
- Omega-3 Fatty Acids: Emphasize the role of EPA and DHA in modulating inflammation and improving meibum quality for dry eye relief. Dosage recommendations.
- Curcumin/Turmeric: Anti-inflammatory properties and its potential role in managing ocular inflammation.
- Vitamin D: Link to immune modulation and overall autoimmune health.

Premium Omega-3 (High EPA/DHA)
Essential for reducing systemic inflammation and managing RA-related dry eye symptoms.
Importance of Interdisciplinary Care (Rheumatologist and Ophthalmologist)
- Stress the absolute necessity of close collaboration between the rheumatologist (managing systemic RA) and the ophthalmologist (managing ocular complications). Explain how seamless communication ensures optimal treatment and monitoring.
Lifestyle Adjustments: Hydration, Environment, and Eye Protection
- Tips for managing dry eye symptoms: humidifiers, avoiding fans/AC, protective eyewear, blink exercises.
❓ Frequently Asked Questions (FAQ) about Rheumatoid Arthritis Eye Complications
How common are eye problems in people with Rheumatoid Arthritis?
Answer: Eye problems are remarkably common, with studies showing that nearly 25% of patients will experience some form of Rheumatoid Arthritis Eye Complications. The most frequent issue is Keratoconjunctivitis Sicca (dry eye), which affects a vast majority of those with systemic autoimmune activity.
What is the most dangerous Rheumatoid Arthritis Eye Complication?
Answer: The most dangerous Rheumatoid Arthritis Eye Complication is Necrotizing Scleritis. If left untreated, it can lead to “melting” of the sclera (the white of the eye) and potential perforation, which is a true ocular emergency that requires immediate systemic immunosuppression to save the patient’s vision.
Can systemic RA medications treat eye-related symptoms?
Answer: Yes, systemic treatments like DMARDs and biologics are highly effective. Because most Rheumatoid Arthritis Eye Complications are driven by systemic inflammation, controlling the underlying disease often reduces the severity of ocular symptoms like uveitis and scleritis.
Why are standard eye drops often insufficient for RA patients?
Answer: Standard over-the-counter drops only provide temporary lubrication. Since Rheumatoid Arthritis Eye Complications involve chronic, immune-mediated inflammation, patients usually require prescription anti-inflammatory drops (like Cyclosporine) or advanced MGD treatments to address the root cause rather than just the symptoms
Can Rheumatoid Arthritis cause permanent vision loss?
Answer: While rare if managed early, certain Rheumatoid Arthritis Eye Complications such as Peripheral Ulcerative Keratitis (PUK) or untreated posterior uveitis can cause permanent scarring and vision loss. Regular co-management between a rheumatologist and an ophthalmologist is essential for prevention.
Conclusion: Protecting Vision in the Face of Systemic Disease
Rheumatoid Arthritis Eye Complications represent a critical aspect of managing this systemic condition. From the widespread discomfort of severe dry eye to the sight-threatening emergencies of scleritis and uveitis, ocular involvement demands vigilant monitoring and proactive intervention. By fostering close collaboration between rheumatologists and ophthalmologists, embracing advanced diagnostic tools, adhering to systemic and topical treatment protocols, and incorporating vision biohacking strategies, individuals with RA can significantly mitigate risks. Protecting your vision requires a lifelong commitment to understanding and addressing every facet of your RA, ensuring that your eyes remain healthy and functional despite the systemic challenges.
A Note from the Founder
"I started CVT because eye health is personal to me. After losing sight in my left eye due to a childhood injury and managing high intraocular pressure for decades, I’ve dedicated my life to finding the best ways to protect the vision we have. Every piece of advice on this site is researched with that same level of care and responsibility. Thank you for being here."